EsophagealPH Metry
What is an "impedance pH test"?
An impedance pH test is done to help diagnose whether you have symptomatic gastroesophageal reflux disease.
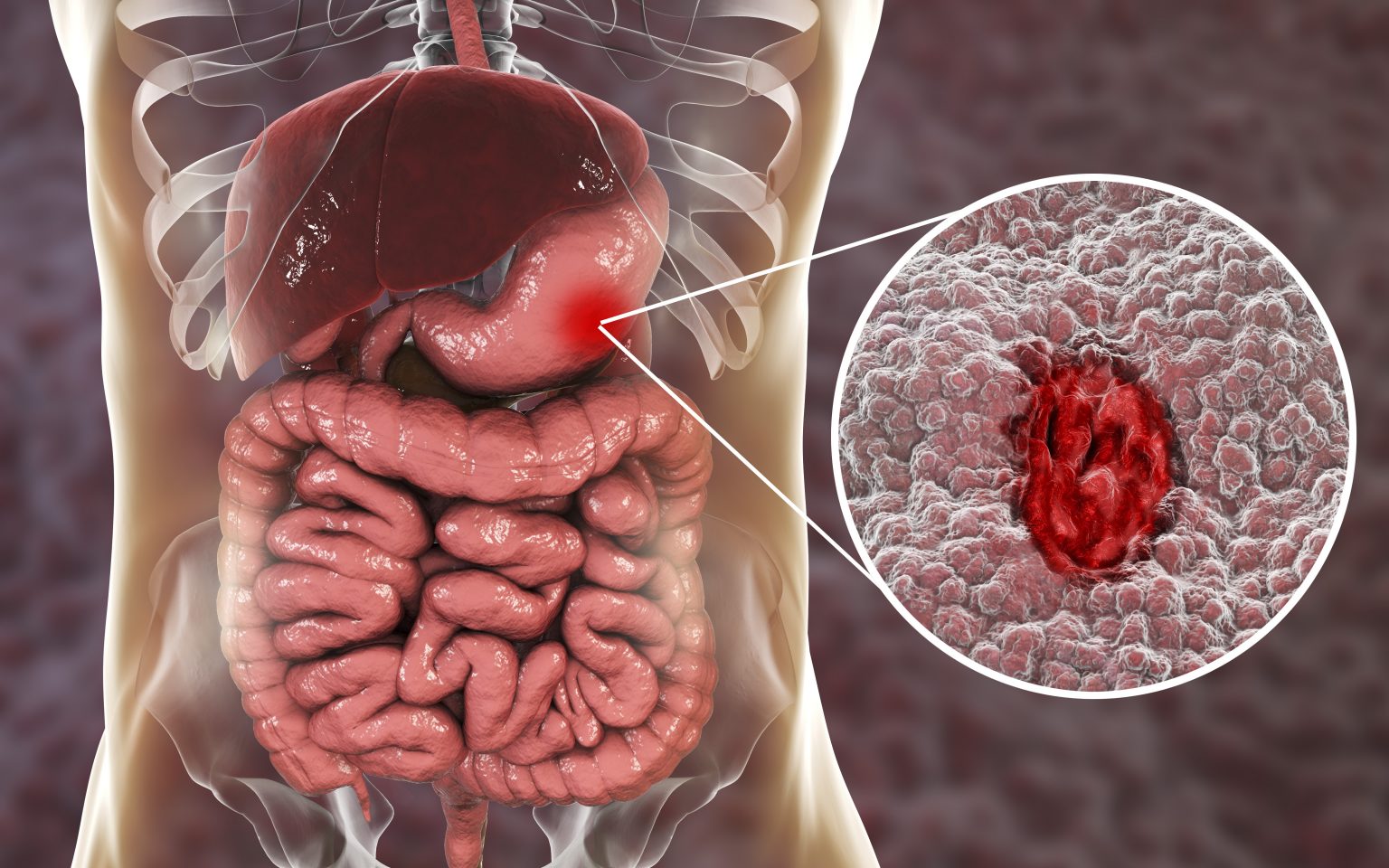
What is "gastroesophageal reflux disease"?
This condition is often called “reflux” or "GERD." Gastroesophageal reflux happens when food and liquid from the stomach back up into the esophagus. This often causes some very uncomfortable symptoms, such as heartburn, chest pain, difficulty swallowing (called dysphagia), a rough-sounding voice, chronic cough, and asthma.
- Gastro refers to the stomach.
- Esophageal refers to the esophagus, the tube that carries food and liquid to your stomach.
- Reflux refers to the reverse movement of the stomach contents up into the esophagus.
- The term “disease” may be used when you have the symptoms at least twice each week, when the symptoms interfere with your daily life, or when your physician can see damage to your esophagus.
What does "impedance pH" mean?
- Impedance refers to something that interferes with what usually happens. In this case, impedance refers to measuring the movement of the food and drink that back up into your esophagus.
- pH refers to the amount of acid in the food/liquids that back up into the esophagus. This measurement is called a "pH level."
How this test works
An impedance pH test uses a small tube called a catheter that has sensors inside it. The catheter is connected to a small device that you wear on your pants or belt. Each time you have a symptom, you press a button on the device that matches that symptom. The sensors then measure how much of your stomach contents (both acid and nonacid) back up into your esophagus. If there is acid in the content, the device also records the amount of acid.
This test may also identify whether or not your symptoms are related to an episode of reflux.
After the catheter is inserted, you may go home or back to your hotel. Over the next 24 hours, each time you have an episode of reflux you are asked to write down the information that’s recorded on the device. You are given a diary to write this information in. Later, you meet with your care team to share the information and to learn more about your condition.
During the procedure
You are seated comfortably during this procedure. A member of your care team may put numbing gel in your nose. The catheter is guided gently through your nose and into your esophagus. The catheter does not interfere with your breathing. While the catheter is moved into position, your eyes may water, and you may gag. You may have a slight nosebleed as well. These are common reactions. Next, your health care provider adjusts the catheter so that the sensors are positioned correctly. (See Figure 1.)
What you need to do
Before you leave the test appointment, be sure you understand how to use the device and what information to write down in the diary.
After the procedure
- Discomfort/pain: Your throat may be sore for a few hours or overnight. A non-aspirin pain reliever with acetaminophen, such as Tylenol™, may help soothe your throat. Follow the package’s dosage instructions. DO NOT use throat lozenges or cough drops while the catheter is in place. You may drink a warm beverage, such as broth, tea, cocoa, or coffee, soon after the catheter is in place. This should soften the tube and make it more comfortable for you.
- Activity: Do not swim, shower, sit in a bath tub, or sing while the catheter is in place. Changes in the breathing muscle when a person sings would interfere with this test. You may do sponge baths as needed. Keep the area around the device dry and clean at all times.
- Diet: While the catheter is in place, do not sip drinks frequently, chew gum or suck on hard candy. You may return to your usual diet when you feel able, unless you are scheduled for additional tests that require a special diet.
- Medications: If you are currently taking medications for gastroesophageal reflux, ask your physician whether you should take these medications during the test. If you are told to not take the medications, you should also avoid over the counter antacids, such as Maalox™, Mylanta™ and Tums™. You may return to your usual medication schedule after the catheter is removed unless otherwise instructed by your health care provider. If the catheter comes out If the catheter comes out accidently, write the time on your log. Coil the end of the catheter (up to the device) in a plastic bag. Return the catheter and device during your scheduled removal appointment. If the device did not capture enough information, a new tube may be inserted
Test results
Talk to the health care provider who ordered the test about how you will learn your results.
When to get medical care?
Most people do not have side effects or problems during the test.
- Some people see a little bit of blood in their saliva for a few days after the test. This is common.
- If you have an uncontrolled nose bleed or extreme pain after the test, go to the nearest emergency medical center.
- If you receive emergency care, on the next business day contact the care team that did your impedance test to update them about your condition.
For more information
If you have questions after reading this information, talk to a member of your health care team.


