Therapeutic ERCP
The following information explains what typically happens during and after an endoscopic retrograde cholangiopancreatography, also called ERCP. If you have questions or concerns about the test or the information in this material, talk to a member of your health care team.
Purpose of the procedure
The purpose of ERCP is to view the inside of the bile ducts and/or the pancreatic ducts to treat blockages, to diagnose disease, to remove stones, or to perform other therapies. The inside of the stomach and duodenum (the uppermost part of the small intestine) may also be viewed during the examination (Figure 1).
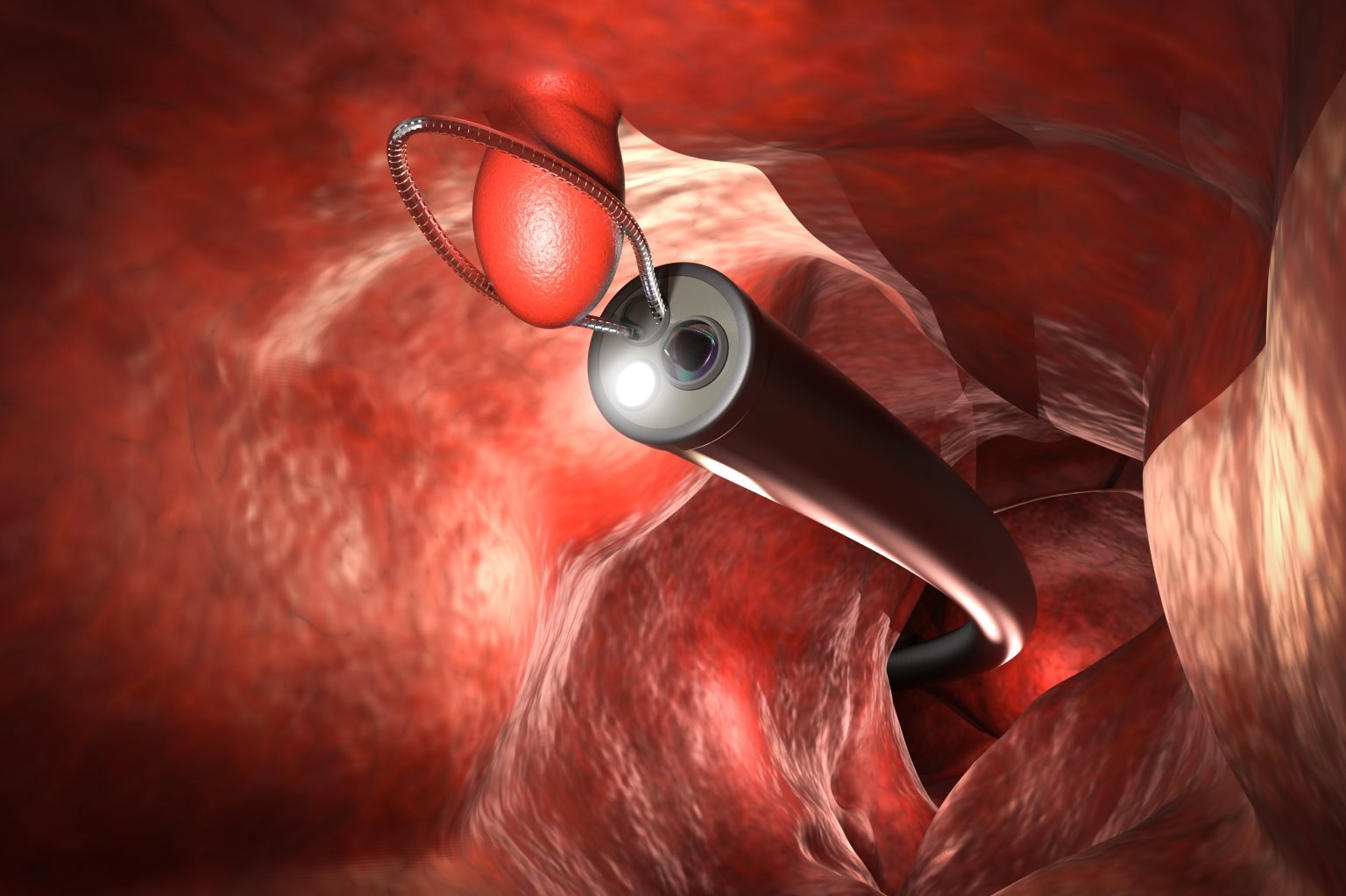
An endoscope (a thin flexible tube) is put into your mouth and passed into your esophagus. The endoscope is equipped with a miniature camera that transmits a picture to a video screen. The endoscope allows the physician to look closely at the upper gastrointestinal tract for ulcers, inflammation and tumors and to find the opening to the bile duct and pancreas duct.
The procedure is also done using X-rays to allow the physician to identify the inside of the bile and pancreas ducts and to monitor passage of instruments from the endoscope to the inside of these ducts.
There is also a channel in the endoscope through which the physician may pass instruments to:
- Inject X-ray dye into your bile duct and/or pancreas duct.
- Obtain biopsy specimens (tissue samples).
- Place drainage tubes (stents) through areas narrowed by scars or tumors.
- Drain cysts.
During the procedure
You will receive medication through a vein, called intravenous (IV) sedation, to help you relax and make you more comfortable. It will make you sleepy. In some cases, anesthesia is given. Antibiotics also may be given through the IV.
You are positioned on an X-ray examination table, usually on your stomach. One or two abdominal X-rays are taken to show the background shadows of your stomach and intestines, intestinal stool and gas.
An anesthetic may be sprayed into your throat to numb it. The physician puts an endoscope into your mouth. The tube does not interfere with breathing. You are monitored throughout the procedure.
You may have a feeling of pressure or fullness as the endoscope is moved or as air is inserted through the tube. The air may cause you to belch.
After the procedure
When your examination is finished, the endoscope is removed and you are taken to the recovery area where you will stay for one to two hours, and occasionally longer. If you are in the hospital, you may be returned to your room right after the examination. If you are an outpatient, you may be hospitalized overnight for observation.
- Effects of sedation: As a result of the sedation you receive, you may have lapses of memory, slowed reaction time, and impaired judgment for 24 hours. For your safety and the safety of others, do not drive for 24 hours after the procedure.
- Do not assume responsibility for young children or anyone dependent on your care. Avoid making important decisions or signing legal documents. Have a responsible adult stay with you for the remainder of the day.
- Discomfort: It is normal to feel bloated, have gas pains and pass gas after your ERCP. Walking may help relieve discomfort from gas pains, which usually last until the day after your examination. Nausea is also common, but should get better within one or two days.
You may have a mild sore throat. Throat lozenges or gargling with warm water may soothe your throat. Non-aspirin pain relievers containing acetaminophen, such as Tylenol™ or generic equivalent in the recommended dose as needed, may help soothe your throat. Blood-tinged saliva for a short time after your examination is normal. Do not be alarmed by this. - Medications: You may resume taking your medications unless otherwise instructed by your health care provider. If you have diabetes or take blood thinners and are unsure about when to resume taking your medications, talk with your health care provider.
- Activity: Rest for the remainder of the day. When you feel you are able, resume your regular activity level, unless instructed otherwise by your health care provider.
- Diet: For the rest of the day, a clear-liquid diet (water, black coffee, clear tea, clear broth, carbonated beverages or fruit juices without pulp like apple and white grape juice) is advised. Your health care provider may advise a more or less strict diet based on your procedure and medical history. Avoid fried or fatty foods, which may increase the risk of pancreas inflammation after the procedure. Do not drink alcoholic beverages for 24 hours. Resume your regular diet when you are able, unless you are scheduled for additional tests that require a special diet.
- Test results: Talk with your health care provider who ordered the test about how to get your procedure results.
Possible risks
Serious complications with ERCP are rare. Inflammation of the pancreas (pancreatitis) is a possible complication. Other possible complications include bleeding and perforation, or tear in the lining of the upper gastrointestinal tract may occur. These complications may require hospitalization and, possibly, surgery. Infection also is associated with endoscopy procedures.
Talk about risks with your health care provider before the procedure. Another risk is a condition called cholangitis. See the boxed text for information about this life-threatening condition.
Cholangitis: A life-threatening complication
Cholangitis is an infection of a bile duct. It is usually caused by bacteria that move up from the place where a bile duct meets the first part of your small intestine. The infection usually happens as a result of something blocking a bile duct.
Early signs can include:
- A fever (can be either low or high-grade).
- Uncontrollable shaking.
- Dark-colored urine or light-colored stools.
- Yellowing of the skin and whites of the eyes, called jaundice.
- Abdominal pain on your upper right side and above your belly button. Most people describe the pain as dull but severe.
Early signs can include:
- Confusion
- Feeling faint or lightheaded.
If you have symptoms of cholangitis, seek emergency medical care immediately. Treatment may include antibiotics, an outpatient procedure or surgery depending on your needs. Do not delay getting help.
When to seek medical help
Seek emergency medical care if you:
- Vomit blood.
- Pass blood in the stool.
- Pass black, tarry stools.
- Have neck or chest pain.
- Experience new, different or continuous abdominal pain — with or without bleeding.
- Develop a temperature of 100.4 degrees Fahrenheit (38 degrees Celsius) or greater.
- Have persistent nausea or vomiting.
- Experience any symptoms that are not improving or are getting worse.
If you have questions about your ERCP, talk with your health care provider. For patients calling after hours, ask for the ERCP doctor on call.
