Constipation
What is Constipation ?
Most people have experienced constipation, a common digestive system problem, at some time in their life. What defines constipation is different for each person. What is normal for someone else may not be normal for you. Many people who report having constipation even have a daily bowel movement. Symptoms you may experience with constipation include:
- Excessive straining during bowel movements.
- Hard stools.
- Infrequent bowel movements (usually fewer than 2 or 3 times a week).
- Inability to empty (evacuate) stool despite the urge to go.
- Passing only small amounts of stool at a time.
- Abdominal bloating, fullness, discomfort or pain.
- A sudden, very strong urge to go.
- Need to manually remove stool with a finger.
Constipation Facts
There are many misunderstandings or misconceptions about constipation. You should know that:
- The normal range can be anywhere from three bowel movements per week to three per day.
- Other things besides constipation may cause abdominal pain.
- You do not need to empty all stool in your colon at one time.
- A bowel movement does not have to happen every day.
- A bowel movement does not have to happen at the same time each day or look the same each time.
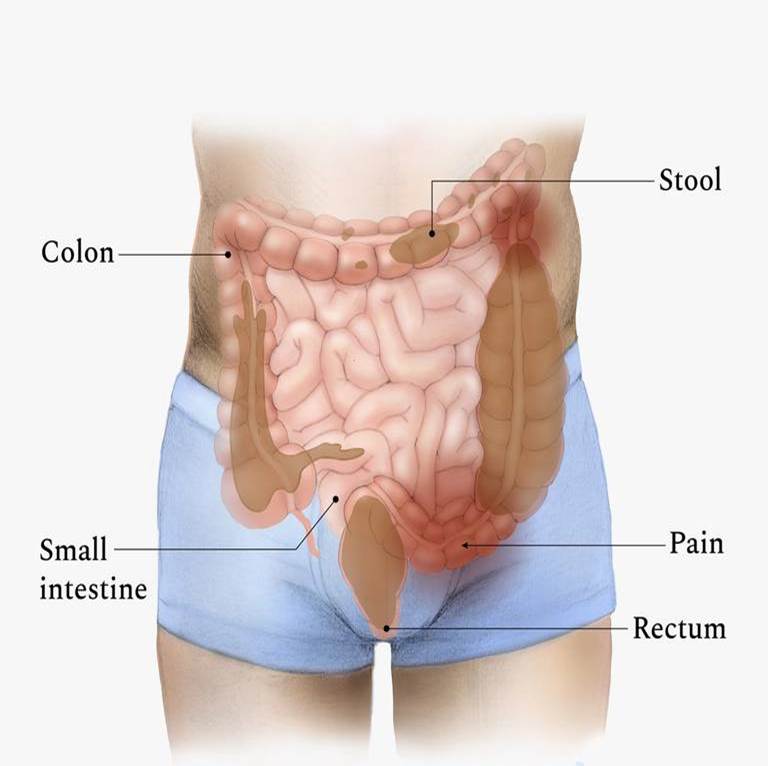
The Colon’s Role
Your large intestine (colon) is located in your pelvic area and lower abdomen and is at the end of your digestive system. It is about five feet long. Layers of muscle line its walls. The muscle contractions produce movement (motility), helping move stool through and out of your body.
The four main functions of the colon are:
- Absorbing water and salts from waste.
- Moving (propelling) waste.
- Storing waste until it is expelled.
- Evacuating waste.
Sometimes stool may move through the intestine at a normal speed (normal-transit) but lack of water (dehydration), medications that slow transit (such as narcotics, antihistamines), certain types of foods, and other conditions may cause the stool to be hard and difficult to pass. Sometimes lack of coordination and inability to relax abdominal and pelvic floor muscles can lead to difficult Colon evacuation. This is called pelvic floor dysfunction.
What are the types of Constipation ?
Constipation causes fall into two main categories: functional and mechanical.
Functional
A functional problem, the most common cause of constipation, is when the bowel is healthy but it is not working the right way. This can happen because of lifestyle choices, such as poor diet, low intake of fiber, not being physically active or even stress. Ignoring the urge to go the bathroom and excessive straining can also be causes.
Pelvic floor dysfunction (dyssynergia) is a common cause of constipation. Pelvic floor dysfunction happens when muscles needed for evacuation do not relax as they should, and involves both abdominal muscles and muscles of the lower pelvis. Both are important for proper evacuation of stool. Sometimes, usually for reasons that are not clear, the muscles do not relax the way they should. Your health care provider and other members of your health care team can help you learn about those muscles and how to retrain and control them.
Constipation is usually manageable. Most people with constipation respond to lifestyle changes. Go to the bathroom when your body urges you to. Try not to wait. Go as soon as you have an opportunity to do so. Avoid excessive straining as it may worsen your constipation in the long term or cause tears or fissures in your anal sphincter, resulting in pain and bleeding. Try to keep a daily routine, particularly in the mornings, and allow enough time in your day to have a bowel movement.
Mechanical
Mechanical causes for constipation are rare and may only contribute partially to constipation. If a mechanical problem is found, medication or surgery may be needed.
Anatomic
Anatomic conditions are caused by abnormal anatomy and may include the following:
- Anal fissure: A small tear in the lining of the anal canal that may develop as a result of passing hard or large stools. Fissures can worsen constipation because the pain may prevent relaxation of the pelvic and sphincter muscles.
- Large hemorrhoids: Hemorrhoids are swollen and inflamed veins in your anus and rectum. If large, hemorrhoids may obstruct stool passage. This is rare. Usually they are small and happen as a result of excessive straining to have a stool.
- Rectocele: Happens when the wall of tough, fibrous tissue (fascia) separating the rectum from the vagina weakens, allowing the front wall of the rectum to bulge into the vagina. Stool enters this cavity rather than exiting the body. It is not uncommon to develop a rectocele when you have pelvic floor dysfunction because of excessive straining.
- Enterocele: A portion of the small intestine can move down and push on the rectum, which causes a blockage.
- Rectal mass (cancerous tumor): A growth in the rectum that may grow so large it keeps you from passing stool normally and comfortably.
- Anal stricture: A tight band of scar tissue at the anal opening that causes difficulty in passing stool. This is very rare and typically only happens because of previous anus surgery or trauma during labor.
Other Causes of Constipation
There are other possible contributors to constipation. These include diseases, which affect the body’s metabolism, internal organs, muscles and nerves. Eating disorders, including anorexia nervosa and bulimia, may also cause constipation. Finally, constipation may be a side effect of medications. Discuss your medications with your health care provider.
How is Constipation diagnosed?
Several tests can be done to find out more about the cause of your constipation so that you and your health care providers can determine the right treatment option for you. You may have one, or more than one, of the following tests:
- Blood tests.
- Anorectal manometry with sensation measures your ability to evacuate stool from the rectum and whether you get the sensation to evacuate.
- Colonoscopy views the inside of the entire large intestine through a miniature camera that is fixed to a thin flexible tube (colonoscope).
- Defecography evaluates the ability to contract and relax pelvic floor muscles and to evacuate stool from the rectum.
- Rectal barastat testing evaluates rectal sensation, capacity, and the ability to contract in response to a meal and medication.
- Anorectal angle exam measures the ability to control and relax the pelvic floor muscles.
- Dynamic magnetic resonance imaging (MRI) evaluates your pelvic floor and other organs during evacuation.
- Flexible sigmoidoscopy views the inside of the lowest part of the colon with a thin flexible tube.
- Electromyography (EMG) tests the electrical activity of the pelvic floor muscles.
Possible Complications
Constipation can be very bothersome. It can make you feel uncomfortable and even irritable. Constipation can also lead to other complications such as hemorrhoids, anal fissures, fecal impaction and rectal prolapse.
Laxatives are sometimes necessary to treat constipation symptoms; however, constant laxative use is not advised. There are many types of laxatives. Discuss laxative use with your health care provider.
How is constipation relieved or treated?
Your health care provider helps develop a plan of treatment just for you. This may include:
- Maintaining a routine in the morning and allowing enough time for a bowel movement.
- Eating a well-balanced diet and having regularly scheduled meals to promote normal bowel function.
- Adding more fiber in your diet by eating more whole grain breads and cereals, fruits and vegetables. Increasing fiber intake gradually minimizes abdominal gas that can be caused by adding more fiber too fast to your diet.
- Increasing your physical activity level, which may stimulate your muscles and aid in regulating bowel movements. Ask your health care provider before you make any drastic changes in your exercise routine; remain active as your health allows.
- Minimizing stress in your life and learning stress management.
- Responding as soon as possible to your body’s need to empty stool, your “call to stool”.
- Retraining your pelvic floor muscles, trying a relaxed body position and using breathing exercises.
If you have questions or concerns about your condition or this information, talk with your health care provider.
