Pelvic Floor Biofeedback 2
What is Pelvic Floor Biofeedback -2?
The Evacuation Disorders Program teaches you the skills you need to make changes that will improve a common medical condition called pelvic floor dysfunction.
The goal of the program is to help you improve control and coordination of your pelvic floor muscles and your ability to pass stool. Many people who complete the program experience improvement in their pelvic floor function.
The Evacuation Disorders Program uses biofeedback therapy and relaxation techniques to teach you how to control your pelvic floor muscles. This is called pelvic floor retraining. The program also helps you identify and change behaviors that may be contributing to pelvic floor dysfunction.
The Evacuation Disorders Program consists of an initial intensive outpatient program and an ongoing home program.
What Is Pelvic Floor Dysfunction?
Pelvic floor dysfunction (dyssynergia) occurs when your pelvic floor muscles do not relax to allow stool to pass from your body.
What are the symptoms of pelvic floor dysfunction ?
These are the most common symptoms of pelvic floor dysfunction:
- Trouble passing stool (straining)
- Feeling that something is blocking the anal outlet when trying to pass stool
- Constipation
- Excessive gas and/or inability to pass gas
- Feeling that there is still stool in your rectum after you have had a bowel movement
- Feeling that you need to pass stool very often
- Need to use laxatives or enemas to help with bowel movements
- A reduced sensation of bladder or rectal urge (you rarely or never feel the urge to urinate or have a bowel movement)
- Leaking urine (especially in women)
- Feeling as though you need to urinate very often
- Difficulty starting urine stream
- Inability to empty your bladder completely when urinating
- Pain and bloating in your abdomen
- Pain in the genital or pelvic area
- Painful intercourse
What are the causes of pelvic floor dysfunction ?
The causes of pelvic floor dysfunction are not fully understood. The following factors may contribute:
- Long-lasting (chronic) constipation
- Sudden (acute) constipation
- Excessive straining to pass stool
- Prolonged episodes of diarrhea
- Fear of loss of stool or urine if muscles relax
- Muscle tension
- Emotional stress
- Physical or sexual abuse
- Childbirth with or without injury to the pelvic floor muscles
- Pain-causing events such as injury, trauma, or radiation to the pelvic area
- Surgery
- Behavioral causes, such as embarrassment of having a bowel movement in a public restroom
To understand pelvic floor dysfunction, it helps to understand what makes up your pelvic floor and how your pelvic floor works with other muscles to pass stool from your body.
Pelvic floor dysfunction in women
Sphincter muscles
Within the pelvic floor are circular muscles called sphincters. These muscles surround the openings to your bladder and rectum. These sphincter muscles control the opening and closing of your urethra and anus.
Pelvic floor muscles
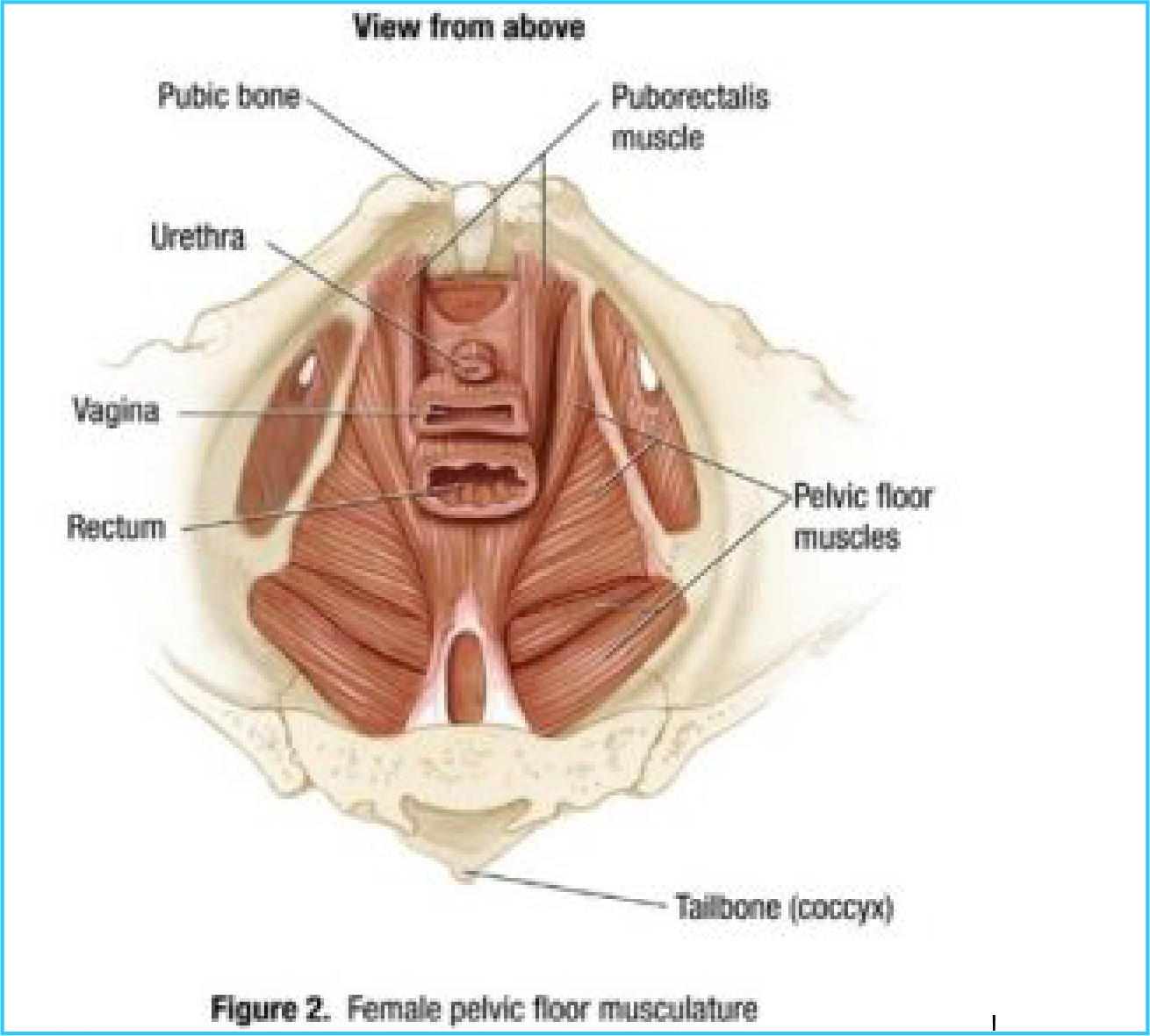
Your pelvic floor muscles are a group of muscles that form the base of your pelvis (Figure 2).
Your pelvic floor muscles attach to your pubic bone in front, your tailbone (coccyx) in back, and your pelvic bone on the sides.
When you look at your pelvic floor muscles from the side, they form a “hammock” of muscles that helps to support your bladder, vagina, and rectum (Figure 3). Your pelvic floor muscles are able to stretch and move up and down.

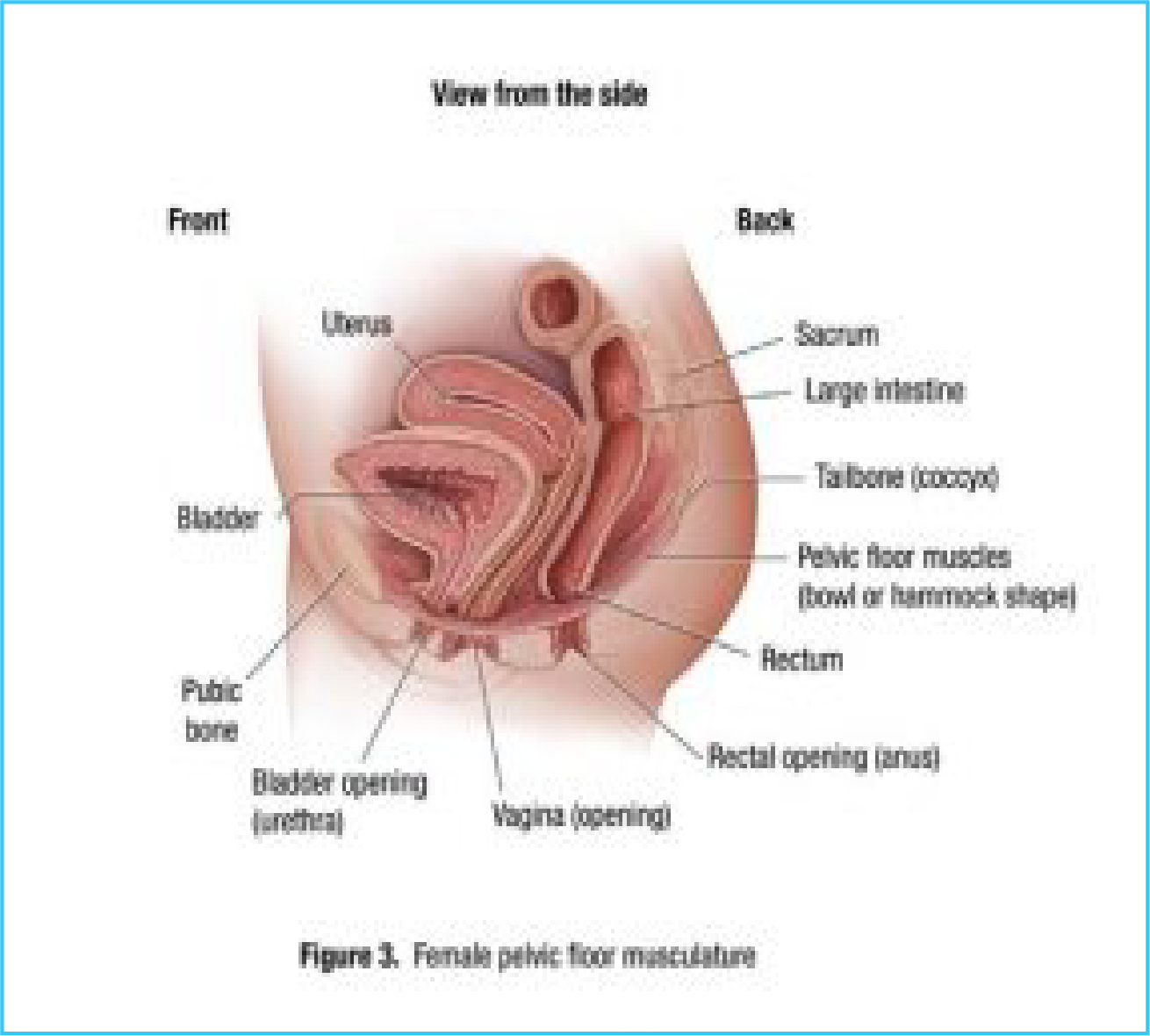
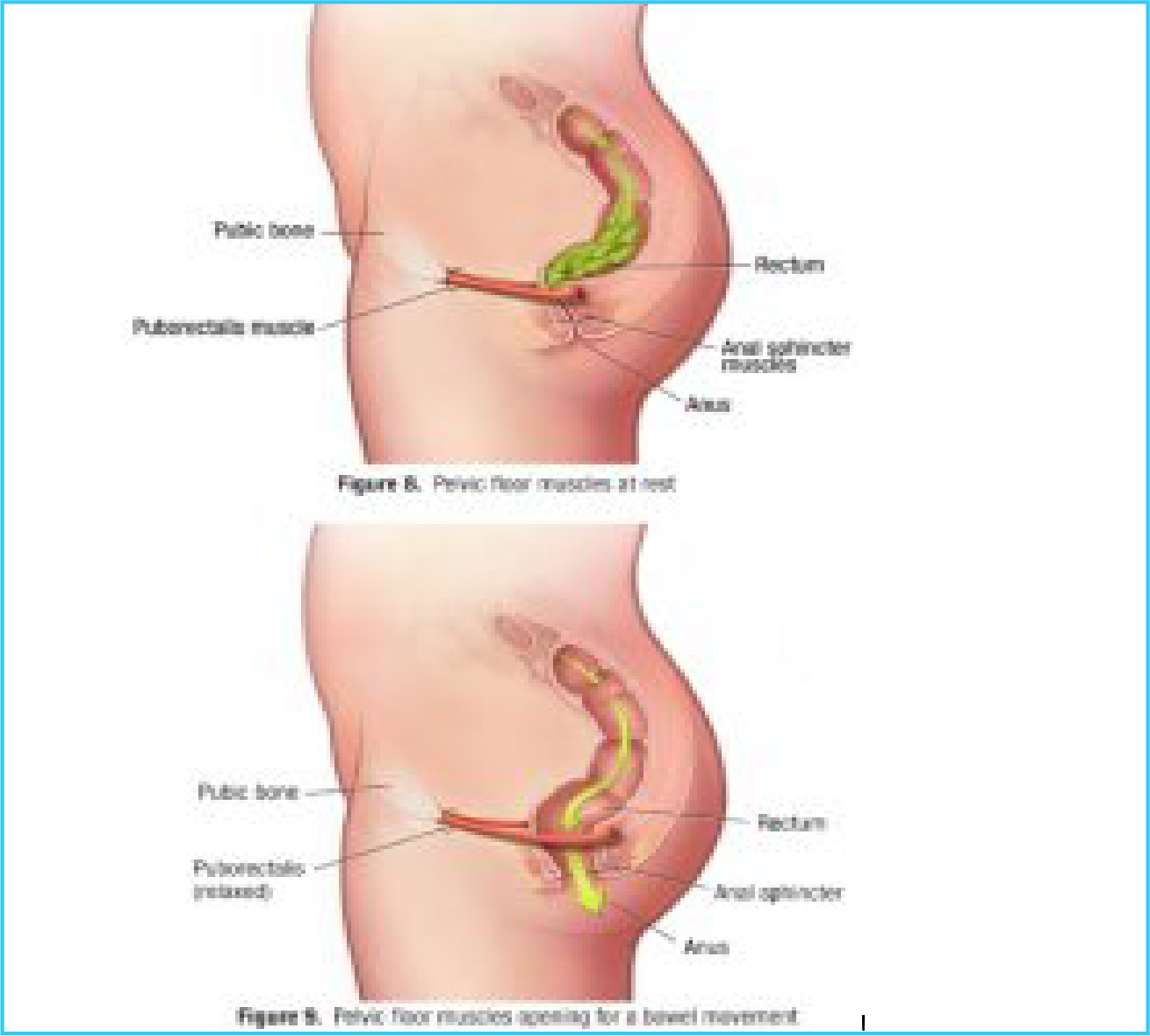
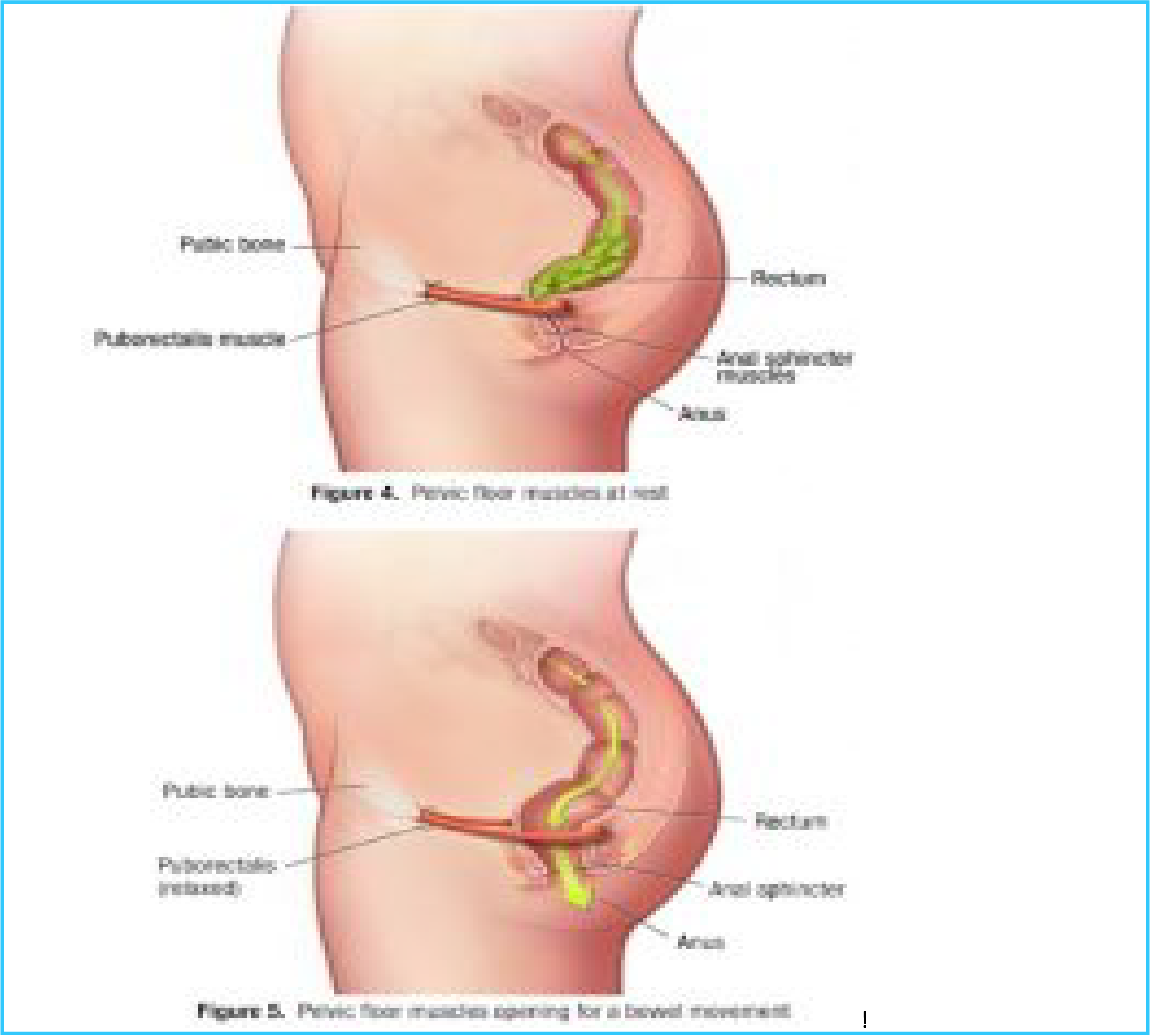
Your puborectalis muscle loops around your rectum like a sling. Pelvic floor muscles at rest are shown in Figure 4. At rest, these muscles are relaxed and the anal outlet remains closed. When you have a bowel movement, your puborectalis muscle relaxes even more. As the anal sphincter opens, stool is easily expelled (see Figure 5).
Normally, the pelvic floor muscles work together to control bladder and bowel functions. When you are ready to urinate or have a bowel movement, your pelvic floor muscles relax and allow you to urinate and pass stool from your body. In women, the pelvic floor muscles also relax to allow for sexual intercourse.
When the pelvic floor muscles do not relax as they should, or when they tighten instead of relaxing, this makes it difficult to pass urine and stool from your body.
This is pelvic floor dysfunction.
Pelvic floor dysfunction in men
Sphincter muscles
Within the pelvic floor are circular muscles called sphincters. These muscles surround the openings to your bladder and rectum. These sphincter muscles control the opening and closing of your urethra and anus.
Pelvic floor muscles
Your pelvic floor muscles are a group of muscles that form the base of your pelvis (Figure 6).
Your pelvic floor muscles attach to your pubic bone in front, your tailbone (coccyx) in back, and your pelvic bone on the sides.
When you look at your pelvic floor muscles from the side, they form a “hammock” or a “sling” of muscles that helps to support your bladder, prostate, and rectum (Figure 7). Your pelvic floor muscles are able to stretch and move up and down.
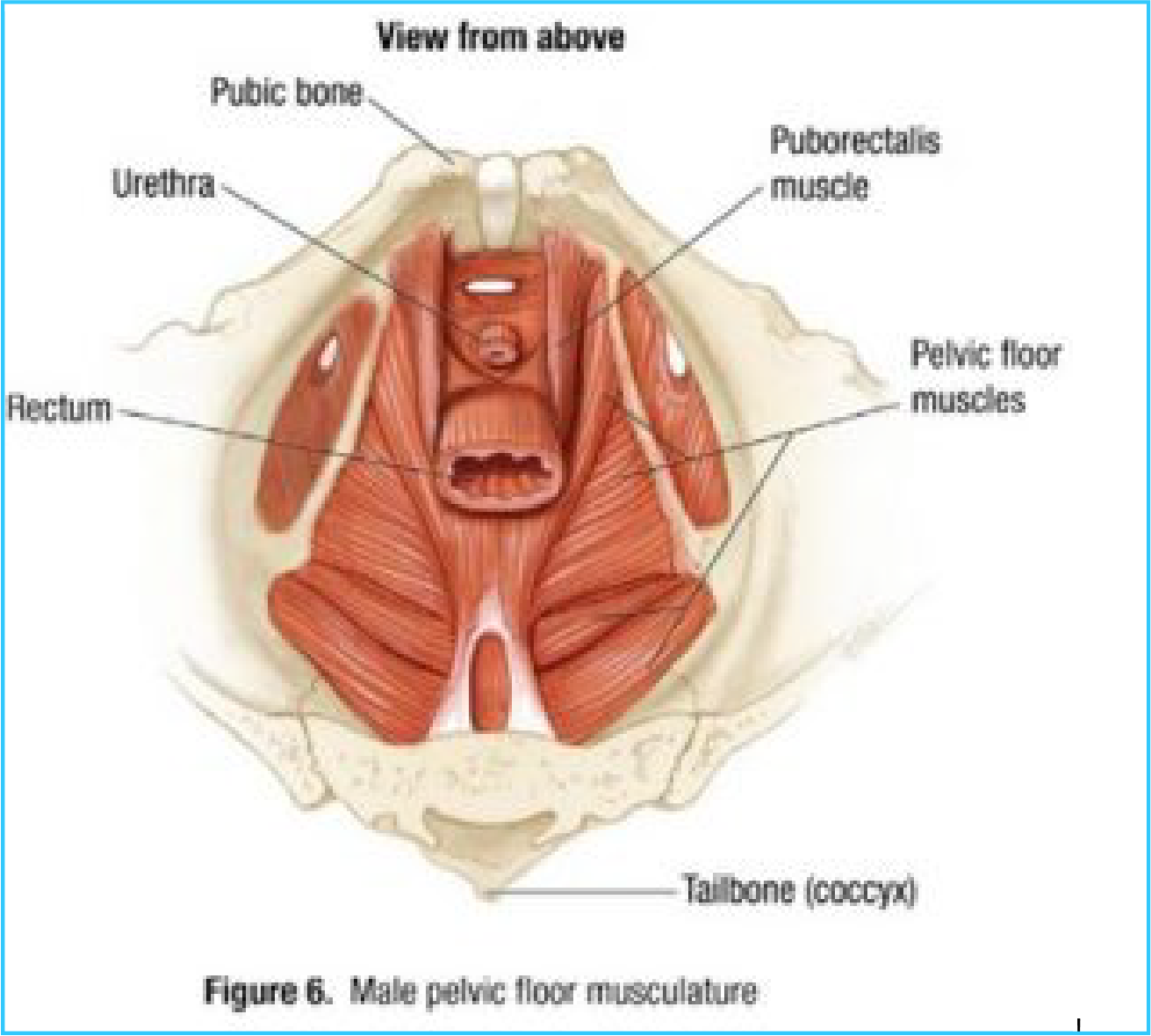

Your puborectalis muscle loops around your rectum like a sling. Pelvic floor muscles at rest are shown in Figure 8. At rest, these muscles are relaxed and the anal outlet remains closed. When you have a bowel movement, your puborectalis muscle relaxes even more. As the anal sphincter opens, stool is easily expelled (see Figure 9).
Normally, the pelvic floor muscles work together to control bladder and bowel functions. When you are ready to urinate or have a bowel movement, your pelvic floor muscles relax and allow you to urinate and pass stool from your body.
When the pelvic floor muscles do not relax as they should, or when they tighten instead of relaxing, this makes it difficult to pass urine and stool from your body.
This is pelvic floor dysfunction.
The mind-body connection and pelvic floor dysfunction You might be surprised to think of having a bowel movement as an act of relaxation. But that’s exactly the right way to think about it. Many people living with chronic constipation spend a lot of time in the bathroom straining to have a bowel movement without good results.
Pelvic floor retraining teaches you to control your pelvic floor muscles. You will learn to allow your pelvic floor to relax rather than strain so that urine and stool can leave your body.
You will learn how to identify the signals that tell you stool has reached your rectum and that you are ready to pass stool.
Your health care team will help you identify behaviours or habits that may be contributing to your pelvic floor dysfunction.
How Your Bowel Works ?
Your colon, also called your large intestine or large bowel, is part of your digestive system.
Your colon processes food waste. It absorbs fluid from food waste and gradually forms it into stool. Your colon stores and removes waste that your body can’t digest. Your colon moves the waste through a series of wave -like contractions called peristalsis. Peristalsis helps to push stool out of your body.
Your colon has four parts (Figure 10):
- The ascending colon is shown in blue. The ascending colon carries waste along the right side of your body.
- The transverse colon is shown in purple. It is the longest region of the colon and is located between the ascending colon and descending colon. It crosses the abdominal cavity from the right side to the left side just below the stomach. Stool formation mostly takes place in the transverse colon.
- The descending colon is shown in red. The descending colon stores waste until it accumulates and is ready to leave your body. When you have a bowel movement, the descending colon helps move stool toward the sigmoid colon and rectum and eventually out of the body.
- The sigmoid colon is shown in yellow. It transports stool from the descending colon to the rectum and anus. Stool is stored in the sigmoid colon until it is ready to be eliminated from your body.
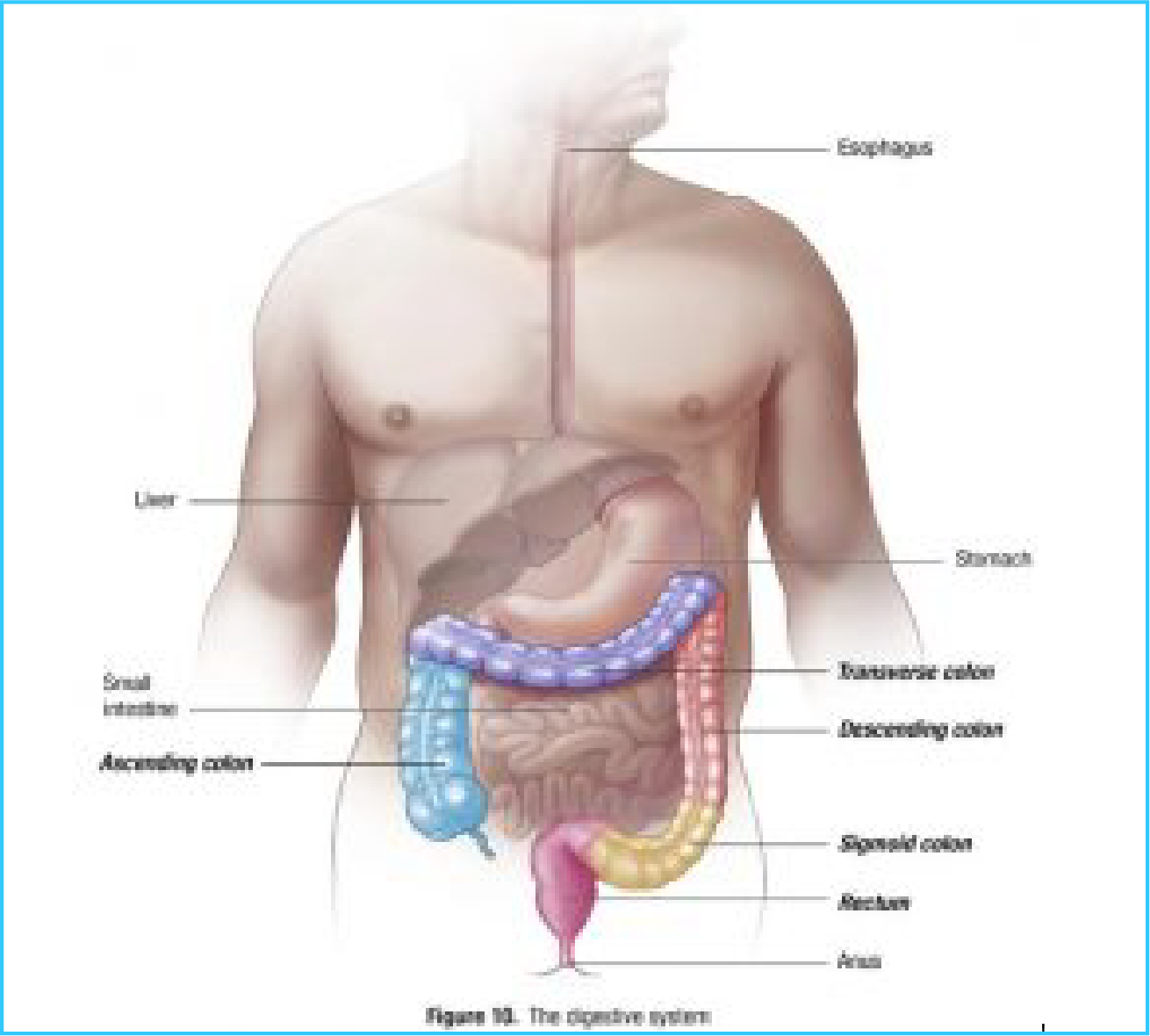
Your rectum is shown in pink. Normally the rectum is empty. Stool does not usually enter the rectum until it is ready to be eliminated from your body.
Passing stool
Like many body functions, normal passing of stool (also called defecation) is a finely coordinated process. Waste moves through your colon into the rectum due to involuntary muscle contractions. You don’t think about these contractions to make them happen. They occur when your colon receives signals that it should move waste out of your body. The more signals the bowel receives, the greater the urge to pass stool.
There are several ways the colon receives signals. Some things that may increase signals sent to the colon include:
- Eating a meal (the larger the meal, the more signals)
- Drinking hot liquid
- Drinking caffeine
- Exercise
The gastrocolic response
Normally, the gastrocolic response (or reflex) is triggered by eating or drinking.
The act of eating stimulates contractions in the colon that help move waste through your bowel.
Don’t skip meals. Eating three meals or six smaller meals each day may help stimulate contractions in your colon.
Biofeedback therapy and relaxation techniques may help your body respond to the signals sent to your colon after eating or drinking.
Bowel problems can occur if your colon is getting too few or too many signals or because you are not responding to the signals.
Normal passing of stool happens when the different parts of your colon work together to propel stool forward and into the rectum (Figure 11).
You begin to feel the urge to have a bowel movement when your body is responding to signals that your rectum is filling with stool. The feeling that you need to pass stool is called a “rectal urge.”
As you sit down to have a bowel movement, your pelvic floor muscles relax and your anal canal opens. This allows stool to pass out of your rectum.
When all is working well, you should not have to strain to have a bowel movement.
When your pelvic floor muscles don’t relax, it may feel as if you need to strain to pass stool from your body. However, straining isn’t helpful for people who have pelvic floor dysfunction. With pelvic floor dysfunction, straining may cause you to tighten the muscles you want to relax.
Pelvic floor retraining will help you learn to relax your pelvic floor to release stool without straining.
What’s normal?
There is no “normal” number of bowel movements. Normal bowel routine is different for every person, and normal may vary from three movements a day to once every three days.
Stool consistency can vary between hard lumps to soft or very loose, often depending on how long the stool has been in the colon and how much water has been absorbed.
Normal stools are comfortable to pass. Ideally, stools should be smooth and formed.
Like many body functions, how regularly you pass stool can depend on a number of things, including:
- Diet
- Medications
- Stress
Your health care team will work with you to address issues that may be causing constipation or diarrhea as part of the Evacuation Disorders Program.
The Evacuation Disorders Program
The Outpatient Program
The Outpatient Program lasts two weeks with appointments typically scheduled Monday through Friday.
You will meet with a member of your health care team two to three times a day the first week and two times a day the second week. You will meet regularly with a nurse who will work with you as you learn to use biofeedback and relaxation techniques to retrain your pelvic floor. You may have appointments with a dietitian. You may also have appointments with a professional who specializes in relaxation.
During the Outpatient Program, you will practice the skills you learn. You will be expected to practice between sessions, in the evenings, and over the weekend. You will report back to your health care team. This will help prepare you for the Home Program.
The Home Program
After you complete the Outpatient Program at Midas, you will continue with a Home Program developed by your health care team. Because each person is different, the length of the Home Program will depend on your needs. The Home Program will help you to continue to improve and use the skills you will learn at Midas.
Getting the most of out of the program
Treatment success depends on you. The best results happen when you are motivated, have an open attitude, regularly practice the skills you learn, and work to change habits that your health care team identifies as contributing to pelvic floor dysfunction.
A commitment to continuing treatment at home, as needed, also is important for success.
Some facts about pelvic floor dysfunction
As you begin treatment, it helps to understand some facts about pelvic floor dysfunction:
- You are not alone. It is a common condition. Many men and women of all ages experience pelvic floor dysfunction.
- There is a mind-body connection with pelvic floor dysfunction, but it is not “all in your head.” It is a real medical condition.
- Pelvic floor dysfunction is not caused by something you consciously choose to do. But you can consciously work to retrain your pelvic floor.
If you have questions or concerns after reading this information, please talk with your health care team.
Using Biofeedback to Treat Pelvic Floor Dysfunction.
Biofeedback therapy can help you learn to control your pelvic floor muscles and change behaviours that may be contributing to your symptoms.
When you are under stress or in pain, your body reacts in ways you don’t even notice.
If you are tense, your pelvic floor may be tense too.
Biofeedback therapy can help you:
- Identify your pelvic floor muscles.
- Isolate your pelvic floor muscles from other muscle groups in your body.
- Tighten your pelvic floor muscles (recognize what tension in your muscles feels like).
- Relax your pelvic floor muscles throughout the day.
- Relax your pelvic floor muscles to release stool and urine.
How biofeedback works ?
Biofeedback gives you the power to use your mind to control your body.
Biofeedback helps you focus on making small changes in your body, such as relaxing certain muscles, to achieve the results you want.
While participating in the Evacuation Disorders Program, you will learn two types of biofeedback using:
- A hand-held biofeedback monitor with a rectal sensor that measures the muscle tension in your pelvic floor.
- A rectal balloon that helps you to retrain your pelvic floor muscles to make having bowel movements easier.
Biofeedback should not hurt. During biofeedback, you’ll practice different relaxation techniques. Your nurse will help you identify strategies to relax your pelvic floor muscles. Biofeedback can help you identify what relaxation feels like for you and what relaxation techniques work best for you.
As part of the Evacuation Disorders Program, you will learn to use the biofeedback equipment and techniques at home on your own.
Remember : A Final Word
The Evacuation Disorders Program teaches you the skills you need to make changes that will improve pelvic floor dysfunction.
If you would like more information about the program, talk to your health care provider.

