Hepatic Artery Embolisation
What is Hepatic Artery Embolization (HAE) ?
This brochure describes hepatic artery embolization and follow-up care. If you have questions about this information, talk with your health care provider.
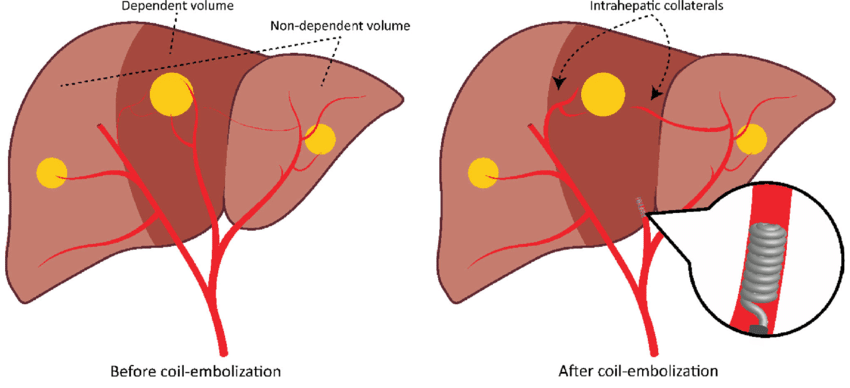
Hepatic artery embolization (HAE) is a technique that blocks blood flow to a tumor by creating a blood clot in an artery (in this case near your liver).
Why is hepatic artery embolization done?
Hepatic artery embolization is used to treat cancerous tumors that cannot be surgically removed. HAE does not cure cancer, but it may shrink tumors and decrease symptoms caused by the tumors
How is hepatic artery embolization done?
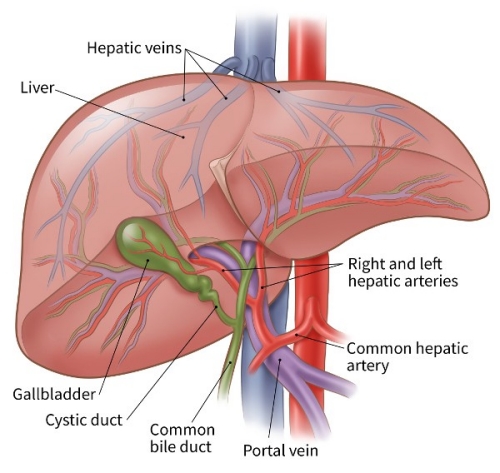
Hepatic artery embolization is done as part of a hepatic artery angiogram. A hepatic angiogram involves inserting a thin, flexible tube (a catheter) through the femoral artery (an artery in your groin) into the hepatic artery (the main artery in your liver).
After viewing the blood flow through the arteries, HAE may be done. A solution is injected through the catheter into the hepatic artery. This creates a blood clot that may slow or stop the flow of blood to the part of your liver that contains the tumor. Slowed blood flow to the area around the tumor may help stop tumor growth and decrease tumor size.
What can I expect before and during hepatic artery embolization?
You will have a physical examination before the procedure. Blood tests and necessary X-rays will be ordered by your health care provider.
You will receive fluids, antibiotics, and appropriate medications through an intravenous (IV) line before and during the HAE. You may receive local anesthetic or numbing medication around the site where the catheter is inserted. During the procedure, you may receive medication that will make you sleepy. Your fluid intake will be closely monitored.
How do I prepare for HAE?
If you have questions about how to prepare for your hepatic artery embolization, ask a member of your health care team.
- If you are in the hospital, your health care team guides you through the process.
- If you are having this procedure as an outpatient, you get written instructions when your appointment is scheduled. Follow the preparation instructions in Section A of your Patient Appointment Guide. If you do not follow the instructions, your appointment may need to be rescheduled.
Plan to remain in the hospital the night of the procedure.
Blood-thinning medications: Before your procedure, your blood-thinning medication routine may need to be changed. Talk with your health care provider who manages these medications as soon as you can. Because blood-thinning medications affect clotting and bleeding, both the health care provider who manages these medications and the provider doing your procedure will need to decide if your medications need to change. For more information on generic and brand name blood-thinning medications, read Blood-thinning Medications and Your Procedure, MC2082-09. If you are not sure if you are on medications that affect blood-thinning, contact your health care provider or pharmacist.
What can I expect after hepatic artery embolization?
You will return to your hospital room after the procedure. You will lie on your back for several hours to allow the catheter insertion site to heal.
Following HAE, you may have nausea, vomiting, upper abdominal pain and fever. You may also have elevated liver function tests and inflammation of the lung lining (pleurisy).
Your physician or nurse will monitor your symptoms and vital signs. You will receive fluids, antibiotics, and appropriate medications through an IV.
After this initial bed rest, you are encouraged to return to your prior level of activity.
Is hepatic artery embolization painful?
Upper abdominal pain is common after HAE. The degree of pain varies from person to person, but it can be severe. Pain medication will be delivered through your IV after the procedure. You also may have nausea and vomiting. Discuss your concerns with your health care provider.
Are there risks?
Although major complications are rare, they can include:
- Liver and kidney failure
- Infection
- Ulcer formation
- Bleeding
- Carcinoid crisis (for people with carcinoid tumors)
- Possibly death
Discuss the risks with your health care provider.
Are there specific instructions for returning home?
Activity restrictions after HAE are:
Up to three days after your procedure, avoid strenuous activities and do not take part in sports.
Do not:
- Lift or move objects that weigh more than 10 pounds.
- Do strenuous exercise (biking, weight lifting, aerobics, golfing).
- Strain.
- Climb stairs.
- Take part in sexual activity.
You may be given instructions about your medication(s), including pain medications.
Avoid alcoholic beverages while taking pain medications.
Bathing
You may shower the morning after your procedure. At that time, you may take off the bandage. For three days after your procedure, do not soak in a tub. Keep the site clean and dry. Do not use creams or powders on the puncture site.
Discomfort
Normally, the site of the puncture is slightly tender and swollen.
area of discoloration or a small knot in the area of the puncture.
puncture site may continue for one to two days.
There may be a small Tenderness at the
You may take a non-aspirin pain reliever containing acetaminophen such as paracetamol in the recommended dose as needed for discomfort.
Medications
Take all your previously prescribed medications, including aspirin, as you normally do unless your health care provider tells you otherwise.
Care for femoral (groin area) sites
If you have active bleeding or swelling of the puncture site:
- Call your designated emergency number.
- Lie down and apply firm pressure with 2 or 3 fingers over the puncture site until help arrives.
- Do not drive yourself to the hospital.
When to call your health care provider
Call your health care provider if you develop:
- Worsening abdominal pain not relieved by pain medication
- A temperature of 100.4 degrees Fahrenheit (38 degrees Celsius) or greater
