Liver Masses
What are Liver Masses ?
This information is intended to help understand liver masses, also called lesions, and how they are diagnosed and treated.
liver mass is a growth in or on the liver. Liver masses can be classified as:
- Noncancerous (benign) masses that usually require no further intervention or observation only.
- Noncancerous (benign) masses that may require further evaluation and treatment.
- Cancerous (malignant) masses that require appropriate treatment.
Most liver masses are noncancerous.
The cause of some types of liver masses can be determined, but for many, the cause is complex and often difficult to identify. Research on the cause and treatment of liver masses is ongoing.
If you have questions about the information in this booklet or your health condition, testing or treatment, talk with your health care provider.
Remember
- Liver masses can be benign or malignant. Most are benign.
- People have a better health outcome when:
- Appropriate and accurate testing is used to diagnose a liver mass as early as possible.
- The type and extent (stage) of the liver mass are accurately identified.
- The liver mass is treated correctly.
- Your health care team consists of multidisciplinary health care providers who are experienced in diagnosing and treating liver masses. Team members may include health care providers from hepatology, gastroenterology, oncology, radiology and surgery.
- After diagnosis, following your health care providers’ instructions for care is important.
Liver Location and Normal Function
The liver is one of the largest organs in the body. It can weigh as much as
4 pounds and is located in the upper right side of the abdomen behind the lower ribs
The liver is like a factory; it performs many tasks essential to the body’s proper functioning. The liver makes substances you need to live and filters harmful materials from the blood. The liver:
- Makes bile, which helps the body digest fat.
- Makes certain amino acids, which are the building blocks of proteins.
- Produces most of the body’s cholesterol.
- Produces urea (the main substance of urine).
- Processes medications.
- Filters harmful substances from the blood, such as alcohol.
- Removes waste products.
- Stores vitamins and minerals.
- Maintains a proper level of glucose in the blood.
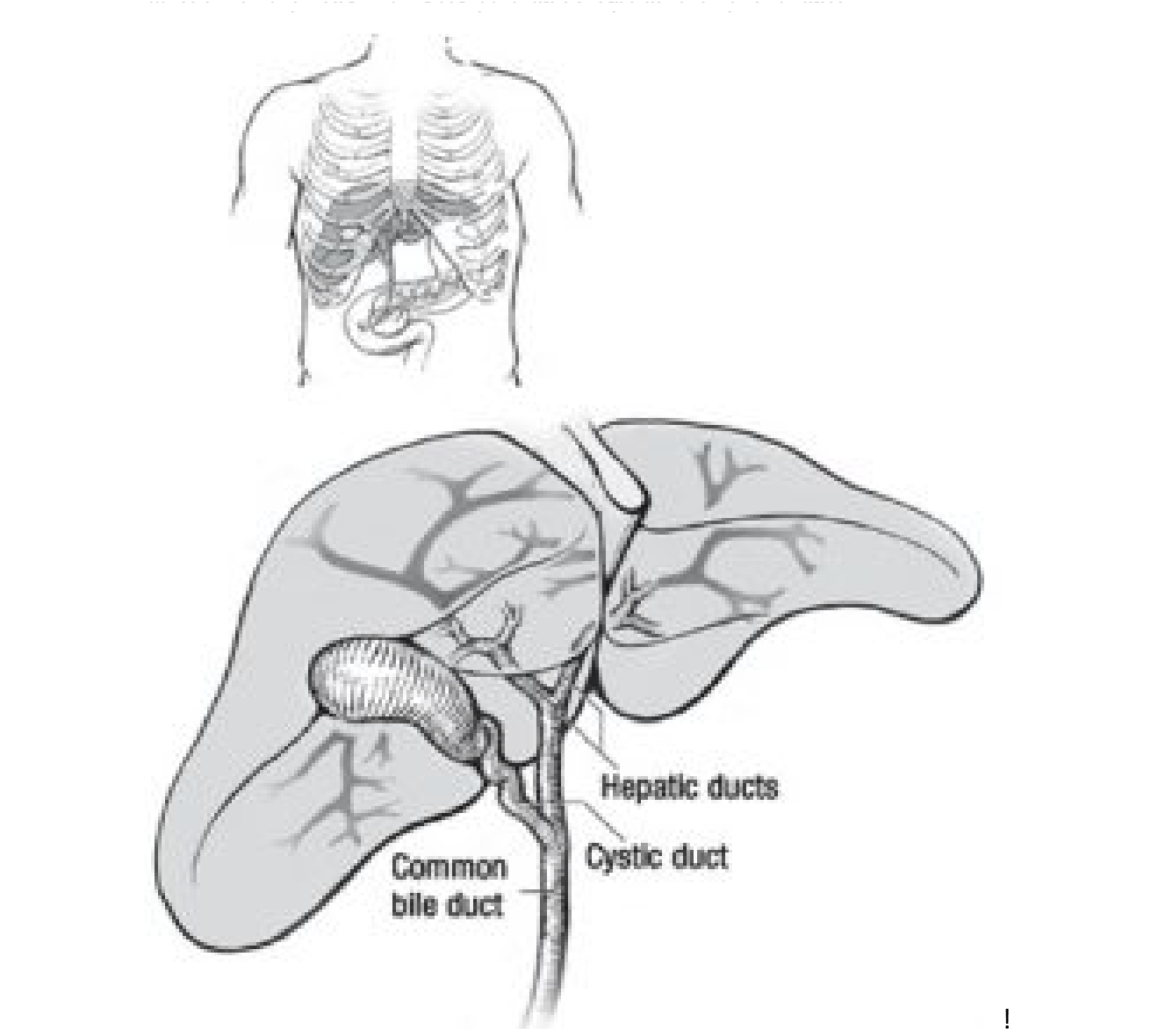
The liver contains many branching structures called bile ducts (Figure 2). These ducts collect bile from the liver for delivery to the intestine. A single large duct, the common bile duct, extends from the liver to the intestine and is connected by the cystic duct to the gallbladder. Bile ducts are lined with small cells called cholangiocytes. Cholangiocytes modify the bile as it passes into the intestine.
How is the diagnosing of Liver Masses done ?
Most liver masses cause no symptoms. They may be found when imaging studies (X-ray, ultrasound, CT scans or MRI) of the abdomen or chest are done for other medical reasons.
However, some liver masses can cause:
- Right upper abdominal discomfort or severe abdominal pain.
- An upper abdominal mass.
- Loss of appetite.
- Involuntary weight loss.
- Low-grade fever and/or night sweats.
- Persistent diarrhoea.
- Anemia (low red blood cell count).
- Yellowing of the skin and whites of the eyes (jaundice), and dark urine.
Medical evaluation
At your examination, the health care provider will talk with you about your medical
history. Tell your health care provider if you:
- Have any of the symptoms listed above.
- Have been diagnosed with cirrhosis or a chronic liver disease, such as hepatitis or primary sclerosing cholangitis (PSC).
- Have other health issues, such as inflammatory bowel disease.
- Drink alcohol or smoke cigarettes.
Your health care provider may ask if you have had imaging studies of your liver, abdomen or chest, and if so, the provider may obtain and review them.
Testing
If you have symptoms of a liver mass, or if a liver mass was found or suspected by another test, more testing may be needed prior to diagnosis or to confirm the diagnosis and identify the type and extent of the mass. Your health care provider may order any of the following tests. Tests other than those listed may also be done.
Blood tests
Blood tests help determine how well your liver is functioning and can check for tumor markers and proteins that increase when cancer is present, a bile duct is obstructed, or the liver is not functioning properly.
Ultrasound with doppler (ultrasonography)
This test uses sound waves to produce pictures of internal organs, including the liver. The test also shows blood flow in the liver. Ultrasound may help provide information about the shape, texture, and makeup of liver masses, and show how close they are to blood vessels in the liver.
As a non-invasive procedure, ultrasound requires no puncture, incision or insertion of an instrument or foreign matter into the body. While you lie on a bed or examining table, a wand-shaped device (transducer) is placed on your body. The transducer sends sound waves into your liver. These waves are reflected back from your liver and displayed on a computer screen.
Computed tomography (also called CT scan or CAT scan)
This test uses X-rays to produce cross-sectional images of your body. Computed tomography can provide information about the size, site and number of masses within the liver as well as surrounding organs. Like ultrasound, computerized tomography is non-invasive. A contrast dye may be injected into a vein during the procedure to help distinguish between different types of masses.
Magnetic resonance imaging (MRI)
MRI creates images using a magnetic field and radio waves. Sometimes a contrast dye also is used. MRI can show an accurate image of the liver and bile ducts.
A needle biopsy of the liver
A needle biopsy may be done to confirm a diagnosis. The biopsy is done by inserting a needle through the skin into the mass. Ultrasound or a CT scan often is used to guide the placement of the needle. Local anesthetic is used at the site of the needle insertion. Tissue is withdrawn through the needle. A pathologist examines the tissue sample under a microscope to make the diagnosis. Rarely, liver mass biopsy does not lead to a diagnosis. In that case, the health care provider’s diagnosis is based on other tests and procedures.
Cholangiogram
A cholangiogram is an X-ray of the bile ducts. Cholangiograms often are done through an endoscope, an illuminated instrument that is inserted through the mouth into the stomach and then into the part of the intestine where the bile ducts drain. Dye is injected into the bile ducts, and X-rays are taken. This procedure is called endoscopic retrograde cholangiopancreatography (ERCP).
Cholangiograms also may be done by inserting a needle through the abdominal wall into the liver and directly into a bile duct. Dye is injected, and X-rays are taken. This procedure is called percutaneous transhepatic cholangiography (PTC or PTHC).
Cholangiograms also can be done by MRI or CT scan.
Positron emission tomogram (PET)
A radioisotope-labeled sugar molecule is injected into a vein in the arm. Later, the liver is scanned to see where the radioactivity has accumulated. Because a mass may absorb large amounts of the labeled sugar, the mass appears as a “hot spot” on the scan.
What are the types of Liver Masses and Their Treatment ?
There are many types of liver masses. The most common are explained in the remainder of this booklet. Also included is a brief explanation about treatment. Treatment for a liver mass varies depending on its type and extent (stage). Talk to your health care provider about any side effects or risks associated with these treatments.
Please note: Your health care provider may recommend a period of observation. This means that your health care provider will monitor your liver mass on a specified schedule. Monitoring may include having blood tests or one or more of the imaging studies listed on pages 4 and 5.
Noncancerous (benign) liver masses
Simple liver cyst
A simple liver cyst is a fluid-filled mass (Figure 3). Having one or more simple liver cysts is common, especially as people get older. Women are more likely to have simple liver cysts than men. Simple liver cysts are also often found when another liver mass is diagnosed. Most simple liver cysts produce no symptoms, but some can grow and cause discomfort.
Treatment
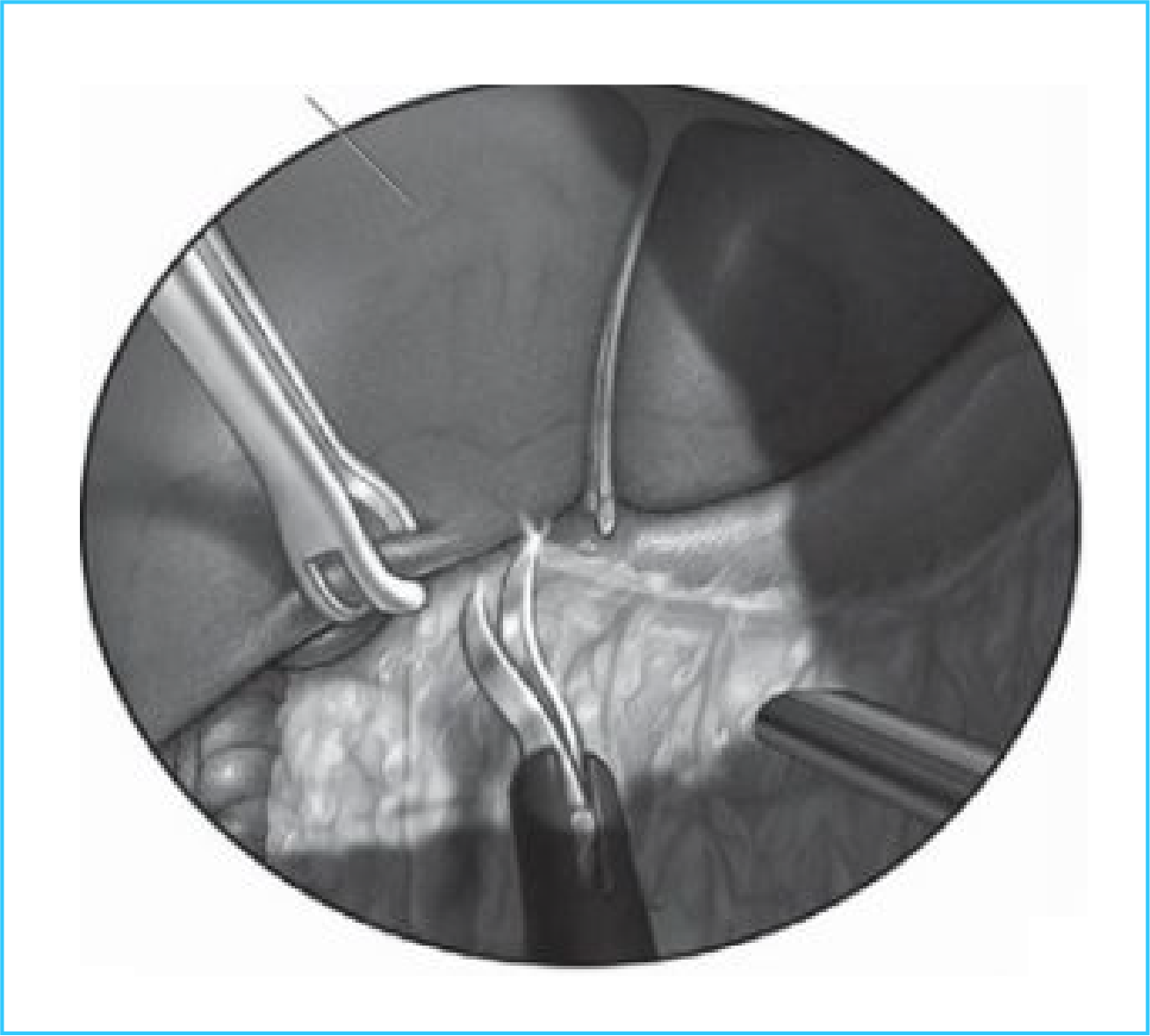
Most simple liver cysts need no treatment. They may go away or remain without changing. However, if a simple liver cyst grows large enough to cause discomfort, your health care provider may recommend that the cyst fluid be drained, or if necessary, the cyst be removed surgically. A laparascopic technique (Figure 4) usually is done to avoid a large incision.
Liver
Cavernous haemangioma
A cavernous haemangioma is a dense tangle of widened (dilated) blood vessels in the liver (Figure 3). Cavernous haemangiomas are second to simple liver cysts as the most common type of noncancerous liver masses. They are diagnosed more often than in the past because the use of imaging studies continues to increase.
People usually have only one, small cavernous haemangioma inside the liver. Sometimes, however, a cavernous haemangioma is large, or a person has several of them. Women are more likely to have cavernous haemangiomas than men.
Most cavernous haemangiomas cause no symptoms, and usually are found when imaging studies of the abdomen or chest are done for other medical reasons. Cavernous haemangiomas can grow and cause abdominal discomfort and put pressure on nearby organs.
Treatment
Most cavernous hemangiomas need no treatment other than observation, as determined by your health care provider. However, if a cavernous hemangioma causes symptoms or grows large enough to cause discomfort, your health care provider may recommend surgically removing the cavernous hemangioma.
Focal nodular hyperplasia (FNH)
Focal nodular hyperplasia is a common benign liver mass that is a localized response of the liver tissue to an underlying congenital malformation of the arteries and veins (Figure 3). People may have one or more FNH masses inside the liver. Women, especially those of childbearing age, are more likely to have a focal nodular hyperplasia than men. What causes these masses is unknown. Most focal nodular hyperplasias cause no symptoms, but some can grow and cause discomfort.
Treatment
Most focal nodular hyperplasias need no treatment other than observation, as determined by your health care provider. However, if a focal nodular hyperplasia grows large enough to cause discomfort, your health care provider may recommend surgically removing it.
Hepatic adenoma
Hepatic adenoma is an uncommon benign mass inside the liver caused by abnormal growth of liver cells (Figure 3). Women, especially those of childbearing age, are more likely to have a hepatic adenoma than men. There appears to be a strong association between the use of oral contraceptives and the development of hepatic adenomas. Hepatic adenomas also occur in people who have certain medical conditions or take certain medications.
Hepatic adenomas can grow and rupture, causing pain, bleeding and other medical problems. Unlike other benign liver masses, hepatic adenomas sometimes can develop into cancerous liver masses, although most do not.
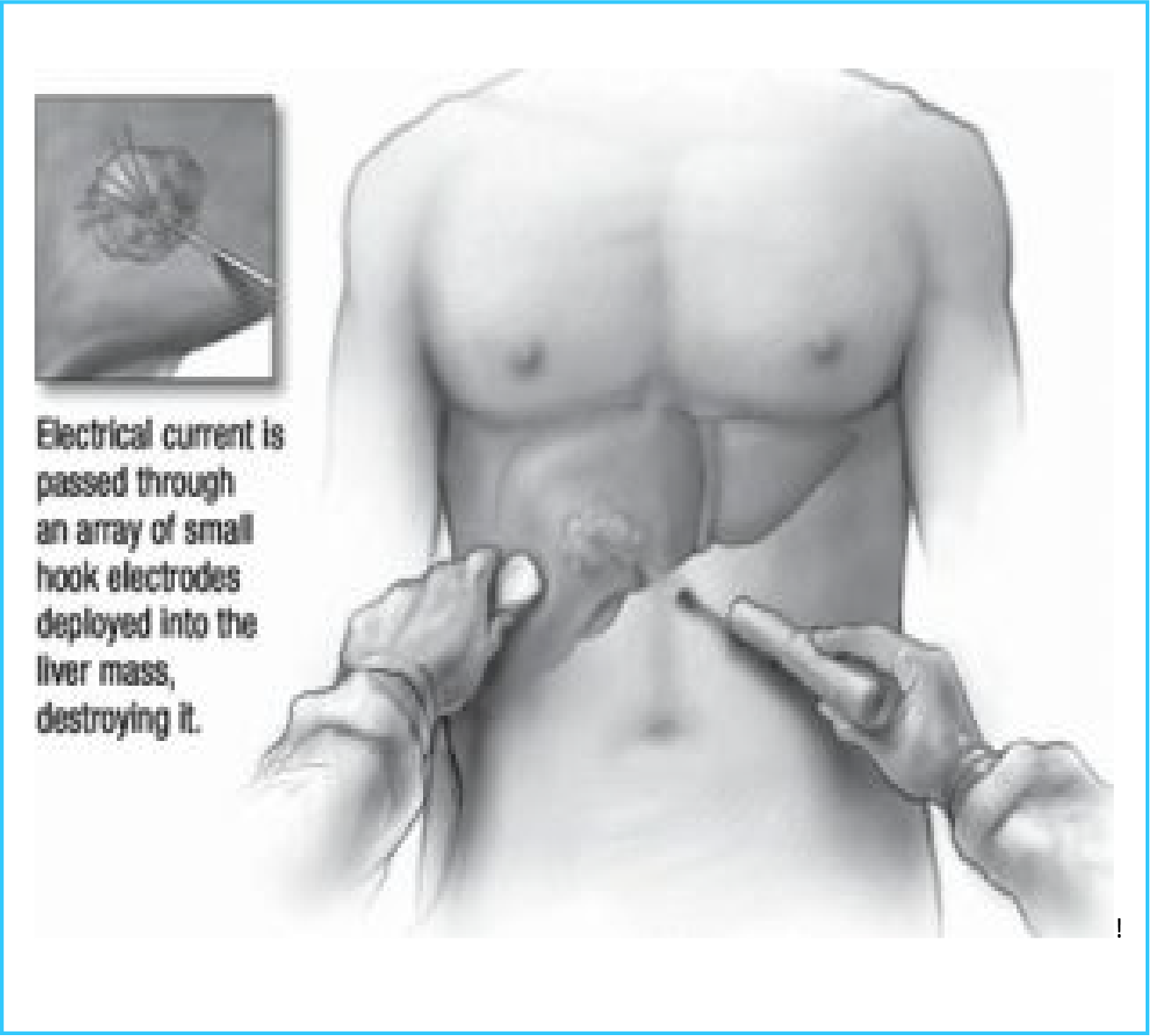
Treatment Hepatic adenomas require further evaluation and treatment. Treatment usually involves surgical removal or ablation (Figure 5) of the hepatic adenoma. During the ablation procedure, a needle electrode is inserted into the mass. Small hook electrodes are sent into the liver mass through the needle. An electrical current is passed through the electrodes into the liver mass to destroy it. Talk to your health care provider about the surgical or ablation procedures.
Cancerous (malignant) liver masses
Hepatocellular carcinoma
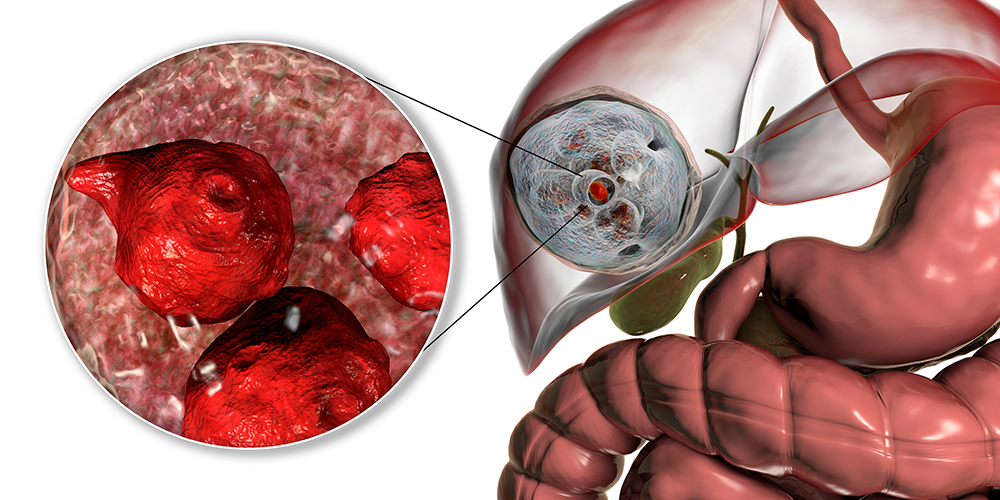
Hepatocellular carcinoma is a cancer that develops in the liver cells (Figure 6). It is a primary cancer of the liver (malignant hepatoma), which means it originates in the cells of the liver and does not come from a cancer somewhere else in the body.
Hepatocellular carcinoma is one of the most common cancers in the world. Most often, it occurs in people who have cirrhosis from viral hepatitis (hepatitis B and hepatitis C), alcohol use, or liver inflammation from fatty liver disease. Other, less frequent causes are hereditary hemochromatosis, Wilson’s disease or primary biliary cirrhosis. Although anyone, at any age, can develop hepatocellular carcinoma, men over 40 years of age are at greatest risk.
Intrahepatic cholangiocarcinoma
Intrahepatic cholangiocarcinoma is a rare cancer that starts in the cells lining the small bile ducts in the liver (cholangiocytes) (Figure 6). Like hepatocellular carcinoma, intrahepatic cholangiocarcinoma is a primary cancer of the liver.
Liver metastases
Metastases or metastatic cancer in the liver occurs when cancerous tumors from other parts of the body spread (metastasize) to the liver. Cancers that commonly spread to the liver include colon, pancreas, lung, gallbladder and breast.
Treatment
Treatment for cancerous liver masses (tumors) depends on factors such as:
- Size and location of the tumor.
- How well the liver is functioning.
- Whether the tumor has spread to other organs or has involved adjacent blood vessels.
- Other specific health-related issues (age, overall health).
- Stage of the cancer.
Treatment can be curative or palliative. Curative treatment is intended to cure the cancer. Palliative treatment is meant to make you feel as comfortable as possible and/ or slow the cancer’s progression when there is no chance for a cure.
Talk to your health care provider about the following treatments for cancerous liver masses, as well as side effects or associated risks.
Surgery
Surgery may involve either removal of the tumor, or for certain conditions, liver transplantation. Surgery may be done through a laparoscope or an open incision into the abdomen. Laparoscopy, which is less invasive and requires smaller incisions, may not be an option because of certain medical or technical reasons.
Surgery may require removal of the bile ducts or part of the liver along with the bile ducts. The liver grows back (regenerates), so that partial removal of the liver poses no long-term health consequences.
Bile may be drained from the liver by using a loop of intestine sewn to the remaining bile ducts.
Possible complications of surgery include leakage of bile into the abdomen, infections, and hernias at the incision site. Tumours can return after surgery.
Liver transplantation may be an option if the tumour is a certain size and has not spread outside the liver. Tumours can recur after transplantation.
Radiation therapy
In cases where surgical removal of liver tumours is not an option, radiation therapy may be used to treat liver tumours. Radiation therapy uses high-dose X-rays to destroy cancer cells and shrink tumours.
Radiation may come from a machine outside your body, or radioactive materials may be placed into your liver. External radiation can affect healthy tissue it passes through as well as tumours. Internal radiation therapy can be delivered directly to the tumor. This is done by guiding a small catheter into the liver, and infusing the radiation therapy through the catheter. The directed radiation destroys the tumor and preserves healthy liver tissue.
Side effects of radiation can include ulcers, tiredness, nausea and vomiting.
Chemotherapy
Chemotherapy is the use of powerful medications to kill cancer cells. Chemotherapy may be systemic, which means it travels throughout your body in the bloodstream, or regional, which means it is delivered through an artery that supplies the liver. Chemotherapy may be used alone or combined with other treatments.
Side effects of chemotherapy can include tiredness, nausea and vomiting.
Radiofrequency ablation (RFA)
During the ablation procedure (Figure 5), a needle electrode is inserted into the mass. Small hook electrodes are sent into the liver mass through the needle. An electrical current is passed through the electrodes into the liver mass, destroying the mass by heat. Ablation is done as a radiological or surgical procedure.
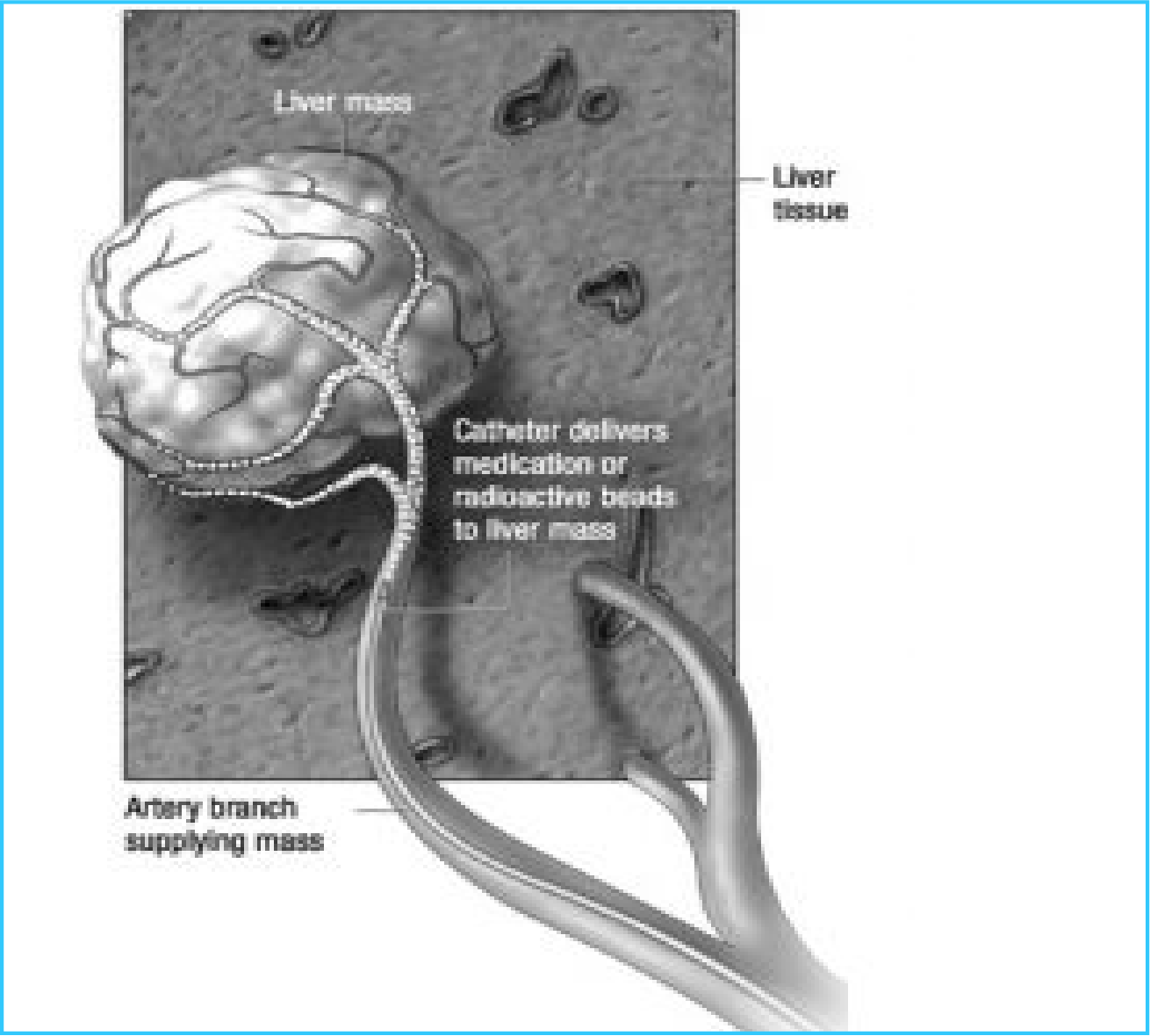
Chemoembolization
Chemoembolization is done by placing a small catheter into an artery in the groin which can be directed into a liver artery that feeds the liver mass (Figure 7). Medication to reduce the growth of the mass and small particles that block the blood supply to the mass are injected into the vessels. This allows delivery of a high concentration of chemotherapy to the mass.
Radioembolization
Radioembolization is a procedure similar to chemoembolization in which radioactive particles in glass or resin beads are injected into a liver artery that feeds the liver mass (Figure 7). The radioisotope usually used for radioembolization is Yttrium 90.
Yttrium 90 radiation projects only a short distance from the beads. Therefore, radioembolization can be done as an outpatient procedure, and special radioactive precautions are not needed.
New treatments
Research shows that all cells transmit or convey information for cell growth, division and death through control mechanisms called signaling pathways. Cancer cells are overly reliant on a few overactive signaling pathways for their growth and spread. These signaling pathways involve enzymes called kinases.
Medications that block the action of these kinases are often used to treat cancers. By blocking the kinase, it is hoped that cancer tumor growth and spread can be controlled. The kinase inhibitor sorafenib is approved by the Food and Drug Administration (FDA) for the treatment of hepatocellular carcinoma.
Contacting Your Health Care Provider If you have questions or concerns about your health, call Midas and ask to talk to your health care provider.

