Portal Hypertension
What is Portal Hypertension ?
This information is intended to help you understand:
- The liver and its function.
- Portal hypertension, also known as high blood pressure in the portal vein of the liver.
- The complications — varices, ascites and hepatic encephalopathy — caused by portal hypertension.
- Signs and symptoms that require immediate medical attention.
- Possible treatment options.
If you have questions about the information in this booklet or your health condition, testing or treatment, talk with your health care provider.
The Liver
The liver is one of the largest organs in the body. It can weigh as much as 4 pounds and is located in the upper right side of the abdomen behind the lower ribs (Figure 1).
The liver is like a factory; it performs many tasks essential to the body’s proper functioning. The liver makes substances that are needed to keep the body alive and filters harmful materials from the blood. The liver:
- Makes bile, which helps the body digest fats.
- Makes certain amino acids, which are the building blocks of proteins.
- Produces most of the body’s cholesterol.
- Produces urea (the main substance of urine).
- Processes medications
- Filters harmful substances from the intestines to prevent them from building up in the blood.
- Removes waste products from the blood.
- Stores vitamins and minerals.
- Maintains a proper level of glucose in the blood.
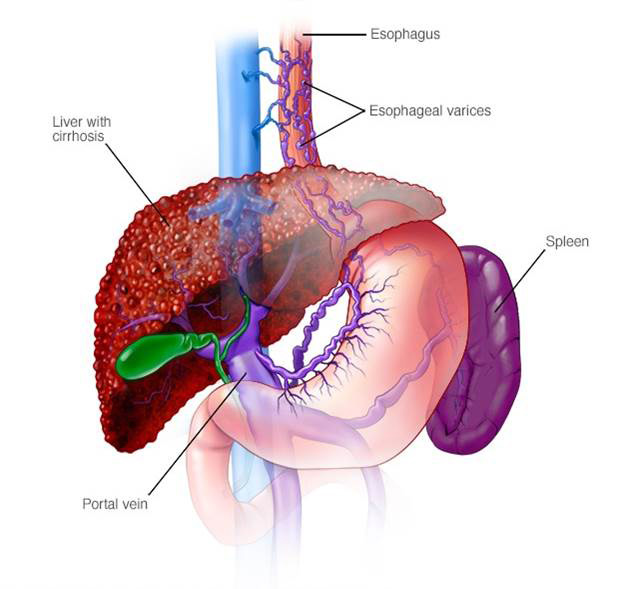
Blood from gastrointestinal organs (esophagus, stomach, intestine, etc.) flows through the portal vein into the liver for processing (Figure 2).
Too much alcohol, viral infections, certain medications, and metabolic or genetic conditions can damage the liver.
Portal Hypertension
To better understand portal hypertension, it may help to understand the process of liver damage.
A damaged liver first becomes inflamed. This condition is called hepatitis (Figure 3b). In some cases of liver disease, excess fat builds up in the liver cells prior to the onset of hepatitis. This condition is called steatohepatitis, also known as fatty liver.
When the damage is more severe and prolonged, cirrhosis of the liver may develop.
Cirrhosis indicates extensive scarring that creates hard nodules in the liver (Figure 3c).
How is Portal Hypertension managed ?
You are an important member of your health care team in managing portal hypertension.
Watch for symptoms of portal hypertension complications and seek medical care as explained on pages 4 to 6.
Help manage your portal hypertension by following your health care provider’s instructions, including:
- Do not drink alcohol. Even a single glass of alcohol can damage your liver further.
- Do not take ibuprofen, aspirin, or aspirin-containing products unless instructed otherwise by your health care provider.
- Take medications needed to control fluid and waste buildup in your body as instructed by your health care provider.
- Follow your schedule for blood tests and medical examinations.
- Eat a low-salt diet, and follow any other diet recommendations from your health care provider.
Varices
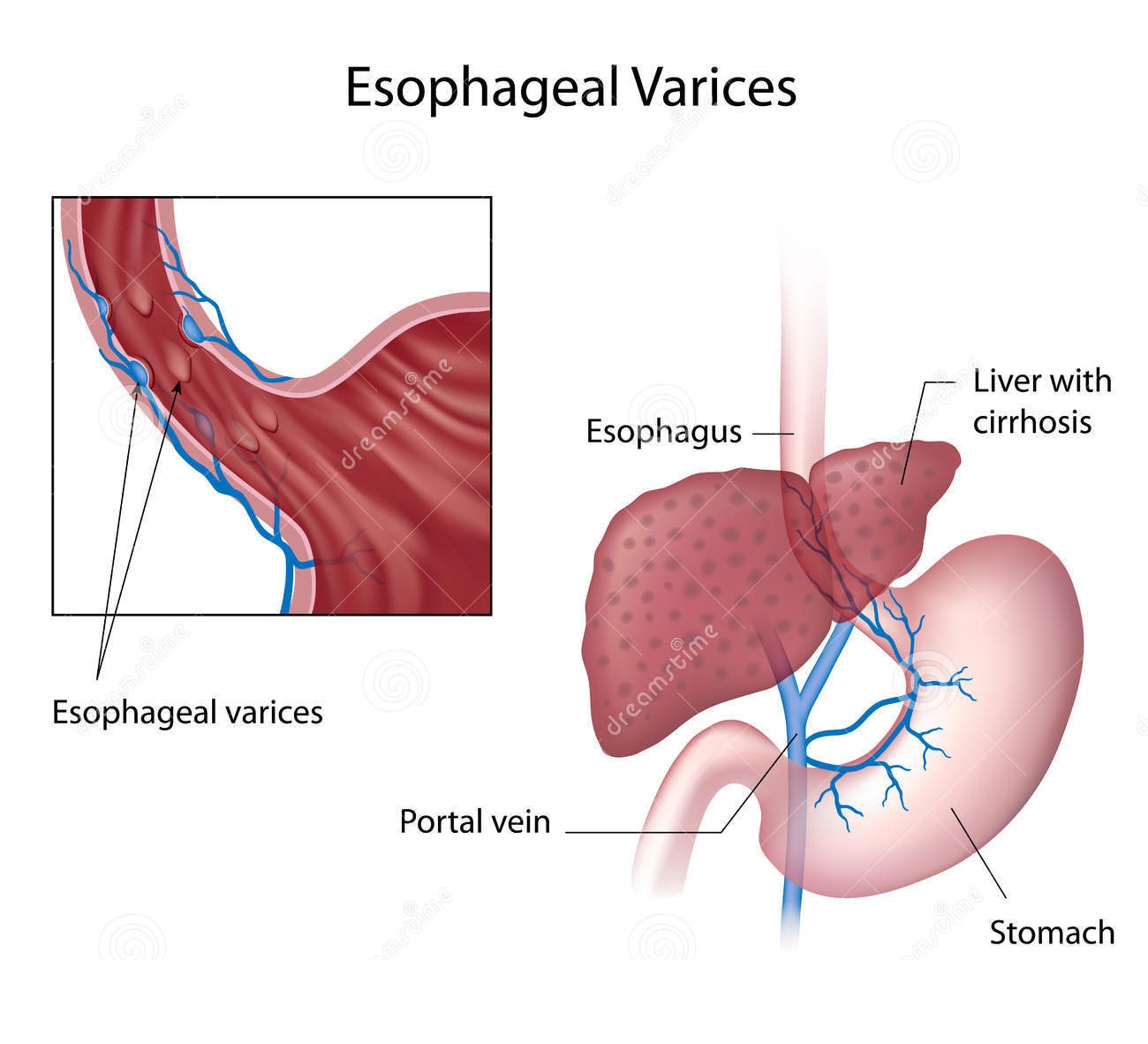
Portal hypertension can lead to high blood pressure in the veins of the esophagus (swallowing tube), stomach and intestines. The pressure causes these veins to enlarge and become twisted. This condition is called varices.
Varices in the esophagus are called esophageal varices. Varices in the stomach are called gastric or stomach varices.
Varices are fragile (thin-walled), which causes a risk of bleeding. When esophageal or stomach varices bleed, blood accumulates in the stomach. Varices typically do not cause pain, even when they bleed.
It is important to know what it means to have varices and to look for signs and symptoms of bleeding varices. Bleeding from broken blood vessels is serious and can be fatal.
Seek medical care
Call your health care provider or go to the nearest emergency medical care facility immediately if:
- You vomit blood or material that is the colour of coffee grounds.
- Your bowel movements contain blood or are black or dark coloured.
What is the treatment for Portal Hypertension ?
Bleeding usually requires hospitalization for treatment. Tests, including upper endoscopy, help determine if the bleeding is from the esophagus or stomach. During an upper endoscopy, a thin flexible tube (endoscope) is guided through the mouth into the esophagus. The endoscope has a camera that transmits pictures of the esophagus, stomach and upper part of the small intestine (duodenum) to a computer.
Talk to your health care provider about treatment options for varices. One option may be to take medications that help prevent broken blood vessels or lower blood pressure in the liver veins.
Another treatment options are endoscopic procedures like variceal banding or endoscopic glue injection. During variceal banding, a lighted tube is passed through the mouth to esophagus (food pipe), and rubber bands or hardened chemicals are placed on swollen blood vessels to block them off. In endoscopic glue injection, a lighted tube is passed into stomach and glue is injected into the gastric varix (swollen blood vessel in stomach) with the help of narrow calibre plastic tube If bleeding cannot be controlled with medication or variceal banding, a procedure called trans-jugular or transvenous intrahepatic portosystemic shunt (TIPS) may be done. With this procedure, blood from the portal vein is rerouted (shunted) to a hepatic vein with a small hollow tube (stent) to decrease the pressure in the varices.
Ascites
When the liver is damaged, the kidneys retain excess salt. The salt holds onto water, and fluid accumulates within the abdominal cavity. This condition is called ascites. The build-up of fluid causes weight gain and swelling of the abdomen, increasing the waistline. Discomfort and breathing difficulty can occur if the abdomen becomes too large. Swelling of the legs also may occur as a result of fluid accumulation.
Seek medical care
Go to the nearest emergency medical care facility immediately if you have:
- A fever.
- Abdominal pain.
- Confusion.
These symptoms may mean that the fluid in the abdominal cavity is infected. This is an urgent situation that requires immediate treatment.
Contact your health care provider if you have a weight gain or loss outside the limits established for you or breathing problems.
Treatment
Follow your health care provider’s instructions about diet, medications and weighing yourself. Your health care provider may arrange for you to meet with a registered dietitian who can instruct you on how to restrict the amount of salt (sodium) in your diet to no more than 2 grams (2,000 milligrams) each day. If you are placed on this diet, it is important to follow it.
You may be given medication, such as spironolactone (Aldactone™) or furosemide (Lasix™), to help remove excess salt and fluid.
If too much fluid collects in your abdominal cavity, the fluid may need to be drained using a needle and a suction device (paracentesis). Talk to your health care provider about this procedure.
What is Hepatic Encephalopathy ?
Some people who have portal hypertension develop a condition called hepatic encephalopathy. When the liver cannot filter waste products from the body, toxins, such as ammonia from the intestines, build up in the brain and affect its ability to function.
Seek medical care
You or your loved one should call your health care provider if you have:
- Difficulty sleeping at night and excessive sleepiness during the day.
- Difficulty concentrating.
- Difficulty with coordination of mental or physical activities.
- Confusion. (This is a symptom of more advanced hepatic encephalopathy.)
If you have these symptoms, do not drive, make major financial decisions, or participate in any activity that could harm you or others. Do not take sedatives or narcotics, or drink alcohol because they can make symptoms worse.
Arrange for a family member or friend to be with you if you have hepatic encephalopathy symptoms because you may not be able to take care of yourself, or your medications, diet and any other treatments your health care provider prescribes for you.
Treatment
Treatment for hepatic encephalopathy requires drinking a medicine called lactulose to rid the intestines of ammonia and other toxins. Work with your health care provider to adjust the dose of this medication to avoid excessive bowel movements or diarrhea.
Your health care provider may recommend that you make changes to your diet.
Liver Transplantation
Varices, ascites and hepatic encephalopathy may be treatable at first. When the liver disease gets worse, the treatments may not work well and a liver transplant may be necessary. Your health care provider may talk with you about liver transplantation.
Contacting Your Health Care Provider
If you have any questions or concerns, contact your MIDAS health care provider.
