Gastroesophageal Reflux Disease
What is Gastroesophageal Reflux Disease?
GERD – A Common Problem
Gastroesophageal reflux disease (GERD) is a common problem that affects many people. One in five people say they have GERD symptoms at least once a week. GERD is often referred to as acid reflux.
As you learn about GERD and its possible treatments by reading this material, think about how you can incorporate the suggested strategies and lifestyle changes.
If you have any questions about this information, talk with your health care provider.
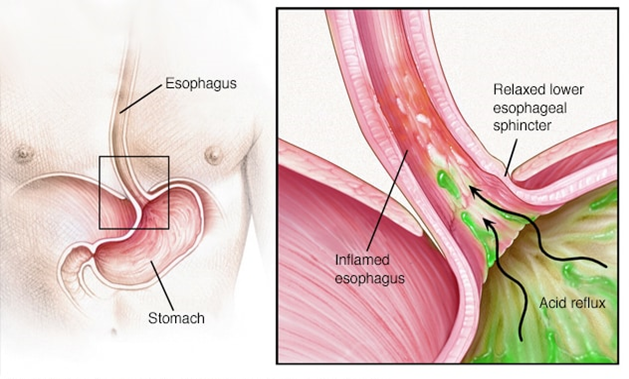
During normal digestion, food or liquid travels from your mouth through a tube called the esophagus into your stomach where acids and enzymes help digest it.
At the lower end of the esophagus is a circular band of muscle called the lower esophageal sphincter (LES). The LES acts as a one-way valve so that food or liquid passes through it but stomach contents are not able to come back up into the esophagus.
If the LES muscle is weak or does not work correctly, for example it relaxes at the wrong time, the contents of the stomach can come back up into the esophagus (reflux). The lining of the esophagus is sensitive to acid and is not protected like the lining of the stomach. This causes troublesome symptoms. For most people, the problem is not that they have too much stomach acid. Rather, the acid goes where it should not be.
When reflux happens often, typically two or more times a week, and interferes with daily life, it usually is considered gastroesophageal reflux disease (GERD).
Other less common reasons for GERD are the lack of saliva or the loss of the esophageal squeeze that can delay the clearing of acid from the esophagus.
What are the common symptoms of GERD ?
Heartburn and regurgitation are the two main symptoms of GERD. Heartburn is a burning feeling that may rise up behind the breast bone. It may be made worse by lying down or eating certain foods. Regurgitation is a feeling of food or fluid coming back up toward the throat. This may cause a bitter taste in the mouth.
Other less common GERD symptoms include sore throat, chronic cough, hoarseness, chest pain, or wheezing.
Hiatal hernia
Some people with a hiatal hernia also have symptoms of GERD. With a hiatal hernia, part of the stomach slides up into the chest and may be associated with a weaker LES. However, although hiatal hernias are common, many people who have a hiatal hernia do not have symptoms of GERD. When GERD symptoms are associated with a hiatal hernia, they are often controlled with medication. Only a small percentage of people who have a hiatal hernia need to have surgery.
How is GERD diagnosed ?
To diagnose GERD, your health care provider asks about your symptoms. If you have typical symptoms that respond to treatment, no other tests may be needed. If your symptoms are not typical or they are concerning, such as unexplained weight loss or trouble swallowing, testing may be needed.
If more testing is needed to diagnose GERD, help determine how severe GERD is, or help with a treatment plan, you may have one or more of the following tests.
Upper endoscopy (EGD)
This test gives your health care team a direct view of the inside of your esophagus, stomach and upper part of the small intestine, especially to look for any damage reflux has done to your esophagus.
During an EGD, a thin, flexible tube with a light and camera (endoscope) is put through your mouth and moved down through the esophagus, stomach and intestine. A sample of tissue may be taken during an endoscopy to test for inflammation. This is called a biopsy.
24-hour pH reflux test
This test measures acid and non-acid reflux of stomach contents that goes into the esophagus.
A thin, flexible tube with acid and non-acid sensors is put through your nose and down your throat into the lower esophagus. It stays there for 24 hours. The sensors measure how often and for how long stomach acid and non-acid goes up into your esophagus.
A second type of pH reflux test measures only acid reflux. For this test, upper endoscopy is used to place a wireless device against the wall of the esophagus. The probe in the esophagus measures stomach acid. After 48 hours of recording, the probe falls off and passes through the stomach and intestines.
Transnasal esophagoscopy (TNE)
This test is done to look for esophageal damage. A very thin, flexible tube with a video camera on the end is put into the nose and passed through the throat into the esophagus. The camera sends pictures to a video screen.
This test is done in the office usually with a local anesthesia medication sprayed in your nose to numb it.
What are the complications of GERD, if not treated ?
Ongoing reflux or reflux not treated effectively can cause the esophagus to become inflamed. The inflammation can damage the esophagus over time and lead to the following complications.
- A sore (ulcer) forms in the esophagus. The sore can bleed causing pain, difficulty swallowing, and anemia.
- The esophagus becomes narrowed into what is called a stricture. This can cause food to stick when you are trying to swallow it.
- Barrett’s esophagus can happen. This condition has no symptoms but needs to be taken seriously because sometimes it can lead to cancer.
Talk with your health care provider about your risk for these complications and what can be done to help.
What is the treatment for GERD ?
The first goal of treating GERD is to have no heartburn or regurgitation. It is not fine to have GERD symptoms a time or two each week. If you continue to have heartburn or regurgitation, you may need additional treatment.
The second goal is to prevent the complications listed previously.
Treatment options for GERD include:
- Lifestyle changes.
- Medications.
- Surgery.
Tell your health care provider if you still have GERD symptoms after trying medication and making lifestyle changes.
Lifestyle changes
Review the following lifestyle changes that are known to help improve GERD symptoms. Select those you want to do to improve the quality of your life.
- Eat smaller meals more often. Do not eat large meals or overeat, especially before.
- Eat slowly and chew food well.
- Stop eating two to four hours before going to bed.
- Stand or sit upright for at least 30 minutes after eating.
- Limit or stop eating foods that bring on your GERD symptoms or make your symptoms worse. Some foods that can cause or worsen GERD symptoms are listed below. You do not need to limit or stop all of the foods listed, only those that bring on or worsen your GERD symptoms.
- Fatty foods, including cream sauces, butter, margarine, shortening
- Fatty meat including high-fat hamburgers, bacon, sausage and ribs
- Chocolate, especially high-fat milk chocolate
- Spearmint, peppermint
- Tomatoes and tomato-based products
- Citrus fruit and juice
- Caffeine
- Carbonated drinks, especially soda pop with caffeine
- Fried foods such as French fries
- High-fat dairy products including whole milk
- Peanut butter and high-fat nuts
- Hot sauces and peppers
- Garlic
- Onion
- Apples
- Cucumbers and pickles
- Green peppers
- Spicy food
- If you smoke, stop. Do not be around tobacco smoke.
- Lose weight if you are overweight. Maintain a healthy weight.
- Limit how much alcohol you drink.
- Do not wear tight-fitting clothes.
- Raise the head of your bed four to six inches. To do this, put blocks or books under the legs at the head of your bed, or place a wedge under the mattress. Sleeping on several pillows increases pressure on your stomach and can make GERD worse.
- When you go to bed, start by lying on your left side to help make it less likely that you will have reflux.
Medications
Your health care provider may recommend that you take medication to help relieve GERD symptoms and to prevent complications of GERD. There are two main types of medication for the treatment of GERD: quick relief and long-term prevention.
Sometimes over-the-counter (OTC) medication is recommended. These include:
- Antacids to neutralize stomach acid. Antacids usually work within minutes to give quick relief for symptoms but they cannot heal an inflamed esophagus damaged by stomach acid.
- Medication to lessen how much acid the stomach makes.
Histamine 2 blockers or H-2-receptor blockers do not act as quickly as antacids but they provide longer relief.
Proton pump inhibitors (PPI) are the most potent blockers of acid and may work for up to 24 hours. A PPI does not stop reflux but it can help relieve symptoms.
If your symptoms are not relieved within a few weeks of taking OTC medications, your health care provider may recommend prescription medication such as:
- Prescription-strength proton pump inhibitor.
- Prescription-strength H-2-receptor blocker, which may be taken for both quick relief and long-acting prevention of symptoms.
- Prokinetic agent to strengthen the lower esophageal sphincter. This medication helps the stomach empty quicker and tighten the valve between the stomach and the esophagus.
Sometimes medications to treat GERD are combined to increase effectiveness.
It is important to follow your health care provider’s instructions and the directions on OTC medication so that the medication works effectively.
All medications may have side effects and risks. Talk with your health care provider about the side effects and risks associated with the medications. One common side effect can be decreased calcium absorption. Talk with your health care provider about having your calcium levels checked.
It may be possible to no longer need medication to relieve GERD symptoms if the lifestyle changes you make stop your GERD symptoms.
Paying for medications to treat GERD
Likely, you will need to take medication to treat GERD for a long time.
Therefore, it is important to plan for how you will pay for medications.
Start by talking with your health insurance provider. Ask them to tell you the cost your insurance covers and the cost you would pay out-of-pocket for the medications your health care provider is recommending that you take.
You also may need to go to several stores to check prices for over-the-counter medications.
If you have questions about medications, talk with your health care provider.
Surgery
Surgery may be recommended if GERD symptoms continue even after making lifestyle changes and taking recommended medications. Surgery also may be recommended if you cannot tolerate the medications, need to have an esophageal sphincter repaired, or have ongoing lung problems such as bronchitis or pneumonia due to GERD.
The surgical treatment for GERD is fundoplication. This treatment gives additional support to the muscles in the lower esophagus to prevent backwash of stomach acid into the esophagus.
There are several approaches to this surgery including:
- Nissen fundoplication. It is done either laparoscopically (several smaller incisions), or open (one larger incision).
- Toupet fundoplication.
- LINX procedure.
- Belsey Mark IV operation.
Talk about each of these surgical approaches with your surgeon. You and your surgeon can decide which approach is best for you.
General anesthesia is used, so you are asleep during the surgical procedure. The surgery usually takes about two to three hours.
Long-term results after surgery are very good. But some people may eventually need to take medication.
If you have questions about the information in this material or would like more information, call the appropriate Midas Clinic telephone number and ask to talk with your health care provider.

